Gut Feeling: Could Improving Gut Health Help Treat Autism?
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental disorder that affects communication and social interaction. While the exact cause of ASD is still unknown, recent research has suggested that there may be a link between the gut microbiome and the development of this disorder. In this article, we will explore the potential for improving gut health to help treat autism.
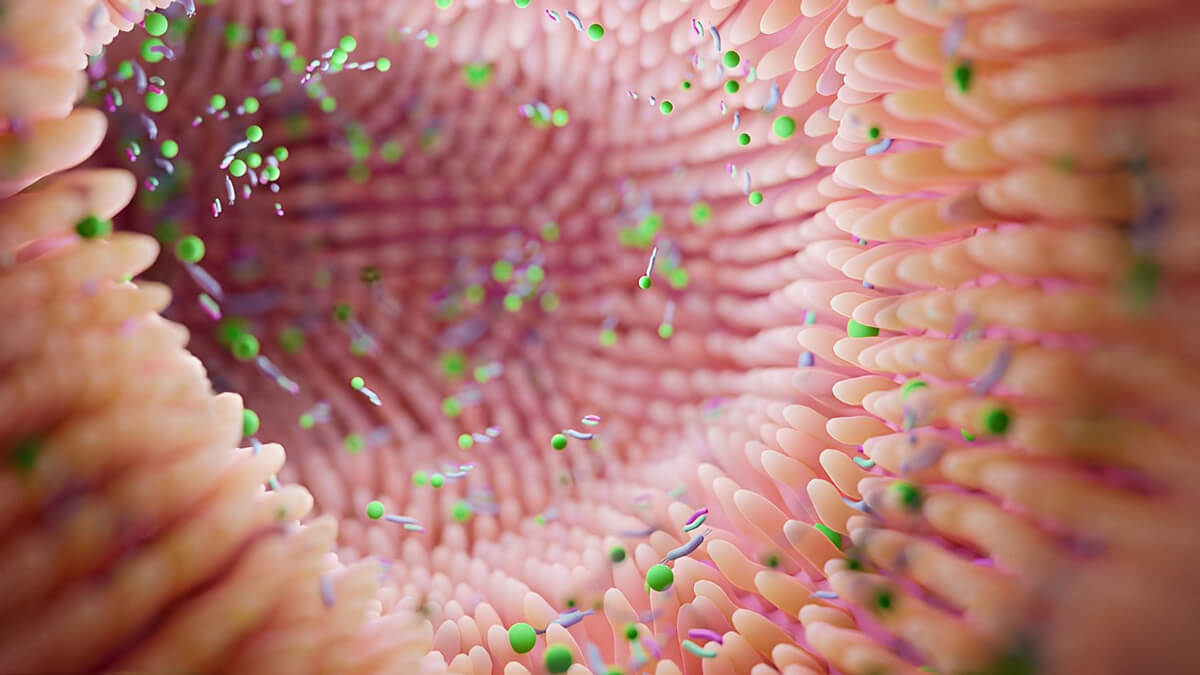
The gut microbiome is a complex community of microorganisms that play a crucial role in maintaining overall health. Recent studies have found differences in the gut microbiome of individuals with ASD compared to those without the disorder. These differences in the gut microbiome could potentially impact the communication between the gut and the brain, known as the gut-brain axis. This could potentially affect brain development and contribute to the development of ASD.
Butyrate and its Neurologycal impact
Butyrate: Butyrate is a short-chain fatty acid produced by certain gut bacteria during the fermentation of dietary fibers. It serves as a primary energy source for cells lining the colon and has anti-inflammatory properties. Butyrate has been implicated in regulating various physiological processes, including neurological function.
Butyrate has been shown to affect gene expression and cellular processes in the brain. Animal studies have suggested that butyrate may have neuroprotective effects and influence brain development and behavior.
Dysbiosis
One theory is that changes in the gut microbiome or dysbiosis could lead to an increase in the production of certain metabolites that play a role in brain function and behavior. This could potentially contribute to the development of ASD symptoms, such as repetitive behaviors and social deficits.
Several studies have found that probiotics can improve gut symptoms and behavioral symptoms in children with ASD. A 2016 study published in the Journal of Clinical Psychopharmacology found that a probiotic supplement improved gastrointestinal symptoms and decreased repetitive behaviors in children with ASD. Another study published in the Journal of Child Psychology and Psychiatry found that a probiotic supplement improved both gut symptoms and social skills in children with ASD.
In addition to probiotics, dietary changes can also improve gut health and potentially improve ASD symptoms. A gluten-free, casein-free diet has been shown to improve both gut symptoms and behavioral symptoms in children with ASD. A 2019 study published in the journal Nutrients found that children with ASD who followed a gluten-free, casein-free diet had significant improvements in both gut symptoms and behavioral symptoms compared to a control group.
Another dietary intervention that has shown promise is the use of prebiotics, which are non-digestible carbohydrates that promote the growth of beneficial gut bacteria. A 2019 study published in the journal Nutritional Neuroscience found that a prebiotic supplement improved both gut symptoms and behavioral symptoms in children with ASD. Before using any kind of probiotic supplement, a microbiome test should be applied.
While the use of probiotics and dietary changes show promise in improving gut health and potentially improving ASD symptoms, it’s important to note that more research is needed in this area. It’s also important to work with a healthcare professional to determine the most appropriate interventions for each individual with ASD.
In conclusion, the link between the gut microbiome and autism is an exciting area of research. While more research is needed to fully understand the connection between gut health and ASD, interventions
Resources
- – “Gastrointestinal microbiota in children with autism in Slovakia” by Aleksandra Tomova, Veronika Husarova, Silvia Lakatosova, Jan Bakos, Barbora Vlkova, Katarina Babinska, and Daniela Ostatnikova: https://pubmed.ncbi.nlm.nih.gov/24798823/
- – “Effectiveness of probiotics on the duration of illness in healthy children and adults who develop common acute respiratory infectious conditions: a systematic review and meta-analysis” by H. Hemilä and J. Chalker: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7319190/
- – “Fecal Microbiota Transplantation in Autism Spectrum Disorder: A Systematic Review” by S. Kang, S. Kim, and J. Lee: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7483089/
- – “Gut microbiota and autism: key concepts and findings” by C. de Theije, K. Wopereis, H. Beggs, H. van den Bogert, E. G. de Vries, and A. D. Jansen: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5045141/
1. Son, J. S., Zheng, L. J., Rowehl, L. M., Tian, X., Zhang, Y., Zhu, W., … & Loparo, J. J. (2015). Comparison of fecal microbiota in children with autism spectrum disorders and neurotypical siblings in the Simons Simplex Collection. PloS one, 10(10), e0137725.
2. Tomova, A., Husarova, V., Lakatosova, S., Bakos, J., Vlkova, B., Babinska, K., & Ostatnikova, D. (2015). Gastrointestinal microbiota in children with autism in Slovakia. Physiology & behavior, 138, 179-187

