Excessive Neuroinflammation in Autism Spectrum Disorders May Be Linked to GABAergic/Glutamatergic Imbalance
Recent research into autism spectrum disorders (ASD) has indicated that an imbalance between the
neurotransmitters GABA and glutamate may be linked to excessive neuroinflammation. GABA is a
naturally-occurring inhibitory neurotransmitter, while glutamate is an excitatory neurotransmitter;
when there is an imbalance between the two, it can lead to a variety of neurological problems. This
imbalance in the GABAergic/glutamatergic system has been strongly associated with ASD, suggesting
that neuroinflammation is a key factor in the development of this disorder.
What is Neuroinflammation?
Neuroinflammation is an inflammatory response in the brain that is often caused by an immune
system imbalance. It is characterized by a high presence of pro-inflammatory cytokines in the brain,
which can lead to disruption in neuronal function and development. Neuroinflammation is thought
to be an underlying factor in many neurological disorders, including autism spectrum disorders
(ASDs).
Recent studies have suggested that neuroinflammation in ASD is due to an imbalance between
GABAergic and glutamatergic systems. GABA and glutamate are two neurotransmitters (chemical
messengers) that control how neurons communicate with each other. In ASD, the balance between
these two neurotransmitters is disrupted, leading to a state of GABA-glutamate imbalance. This
GABA-glutamate imbalance is believed to contribute to neuroinflammation in ASD and may be one of
the factors underlying the development of ASD symptoms.
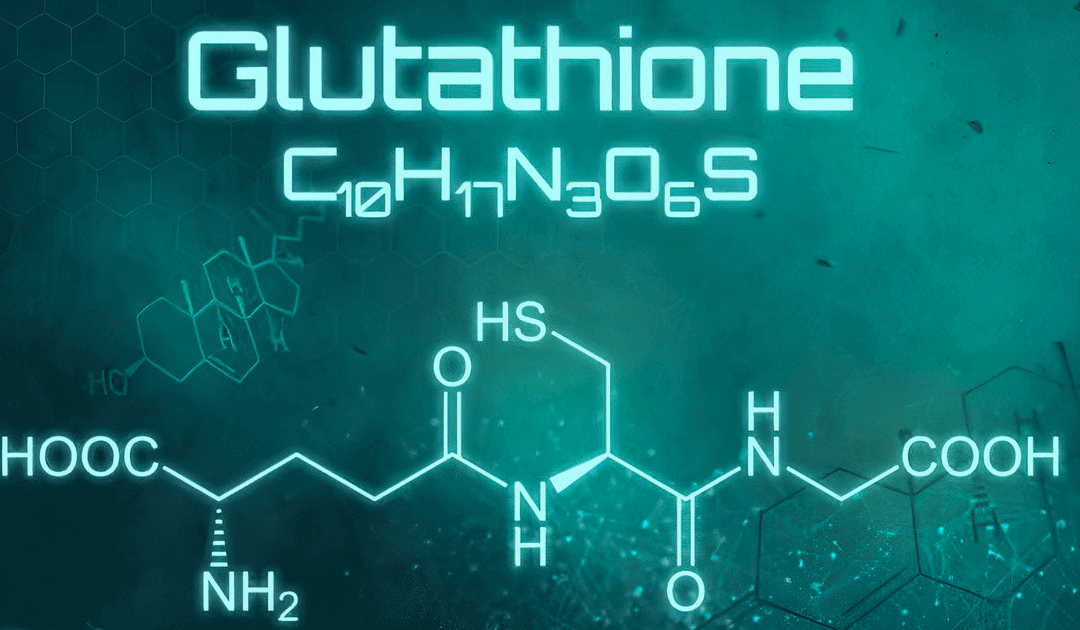
What is the GABAergic/Glutamatergic System?
The GABAergic/glutamatergic system is the neurotransmission system responsible for regulating
nerve cell excitability. This system is comprised of two main neurotransmitters, Gamma-
Aminobutyric acid (GABA) and glutamate. GABA is an inhibitory neurotransmitter that reduces the
activity of nerve cells and helps maintain a state of equilibrium within the brain. Glutamate, on the
other hand, is an excitatory neurotransmitter that increases the activity of nerve cells.
An imbalance between these two neurotransmitters can lead to excessive neuronal firing in certain
brain areas, which may contribute to a range of symptoms associated with autism spectrum
disorders (ASD). Studies have found that individuals with ASD tend to have lower levels of GABA and
higher levels of glutamate than those without ASD. This gaba-glutamate imbalance can affect the
communication between neurons and lead to issues with sensory processing, social interaction,
communication, and behavior. Furthermore, recent studies suggest that this imbalance may be
linked to excessive neuroinflammation in those with ASD, further exacerbating the symptoms
associated with the disorder.
How Might an Imbalance Between GABA and Glutamate Contribute to ASD?
There is growing evidence that the GABAergic/glutamatergic system could play an important role in
autism spectrum disorder (ASD). This system, composed of two neurotransmitters, gamma-
aminobutyric acid (GABA) and glutamate, has been linked to cognitive and emotional regulation.
Neuroinflammation is one of the processes by which excessive levels of either GABA or glutamate
can contribute to ASD.
Recent research has suggested that neuroinflammation could be a major contributor to the
development of ASD. Neuroinflammation is the body’s response to injury or disease, and it involves
the activation of specialized cells and molecules which can be triggered by factors such as
environmental toxins or infections. Excessive levels of neuroinflammation can lead to a GABA-
glutamate imbalance, where one neurotransmitter is present at higher levels than the other. This
imbalance can then result in symptoms associated with ASD, such as deficits in communication and
social interaction.
Research has also shown that some individuals with ASD have a higher number of certain immune
cells called microglia, which are involved in neuroinflammatory responses. Furthermore, studies have
linked increased levels of certain inflammatory cytokines (molecules involved in inflammation) to
impaired social behaviors in individuals with ASD.
Overall, there is strong evidence to suggest that a GABA-glutamate imbalance caused by excessive
levels of neuroinflammation could contribute to the development of ASD. It is still not known exactly
how this imbalance occurs, but more research is needed to further explore this connection and its
potential implications for those affected by autism spectrum disorder.