Autism and Genes, Neuroplasticity
Lithium is often associated with psychiatric medication, but at low doses, a form called lithium orotate is gaining attention for its potential neuroprotective effects. Naturally occurring in trace amounts in water and some foods, lithium plays a role in brain health, mood regulation, and cellular resilience. This article explores how lithium orotate may support cognitive function, emotional balance, and long-term brain health — and how to use it wisely.
What Is Lithium Orotate?
Lithium orotate is a salt of lithium and orotic acid, available as a nutritional supplement. Unlike prescription lithium carbonate, which is used to treat bipolar disorder at high doses, lithium orotate provides lithium in much smaller amounts — typically 1 to 5 mg per day — which may still exert therapeutic benefits with a better safety profile.
Lithium Orotate and Brain: Benefits of Low-Dose Lithium Orotate
1. Neuroprotection
- Enhances BDNF (brain-derived neurotrophic factor), supporting neuron growth and repair
- Protects against excitotoxicity and oxidative stress
2. Mood Stabilization
- May reduce anxiety, irritability, and emotional reactivity
- Supports balanced neurotransmitter activity
3. Cognitive Support
- Improves focus and working memory in some individuals
- May slow age-related cognitive decline
4. Anti-Aging and Longevity Potential
- Animal studies suggest lithium may increase lifespan and reduce age-related inflammation
Mechanisms of Action
Lithium influences multiple cellular pathways, including:
- GSK-3 inhibition: Affects mood, circadian rhythms, and neuroplasticity
- NMDA receptor modulation: Helps balance glutamate activity
- Telomere maintenance: May support cellular aging resistance
Is It Safe?
In low doses, lithium orotate is generally well tolerated. However:
- Long-term use should be monitored, especially in those with thyroid or kidney conditions
- It’s best to consult a healthcare provider before starting, particularly if taking other medications
Suggested Use and Dosage
- Typical dose: 1–5 mg elemental lithium daily (check label carefully)
- Best taken with food
- Start low and observe effects gradually
Final Thoughts
Lithium orotate is a promising tool in the natural mental wellness toolkit. From neuroprotection to mood balance, its broad mechanisms of action make it a fascinating subject of research and practice. While not a substitute for clinical treatment when needed, it may offer gentle yet meaningful support for cognitive and emotional health.
Autism and Genes, Microbiome and Gut health
Is there a link between microbiom and autism? The gut and the brain are more connected than we once thought — and this connection is especially relevant in autism spectrum disorder (ASD). Emerging research highlights how the gut microbiome may influence neurodevelopment, immune regulation, and behavior in individuals with autism. In this article, we explore the complex relationship between gut health and autism and discuss natural interventions that may support improved outcomes.
What Is the Gut Microbiome?
The gut microbiome refers to the trillions of microorganisms residing in the digestive tract. These microbes help regulate digestion, produce neurotransmitters, modulate the immune system, and maintain the integrity of the gut barrier. Dysbiosis — an imbalance in the microbiome — is increasingly associated with neurological and developmental disorders.
Microbiome Differences in Individuals with Autism
Several studies have found distinct differences in the gut microbiome composition of individuals with ASD, including:
- Lower diversity of gut bacteria
- Increased levels of Clostridium and Desulfovibrio
- Reduced beneficial strains like Bifidobacterium and Lactobacillus
These microbial shifts are linked to symptoms such as:
- Gastrointestinal distress (constipation, diarrhea, bloating)
- Irritability, anxiety, and sleep issues
- Increased immune activation and inflammation
How the Gut Microbiome Affects the Brain
The gut and brain communicate through the vagus nerve, immune signaling, and microbial metabolites (like short-chain fatty acids). Disruptions in this gut-brain axis may contribute to neuroinflammation, altered neurotransmitter balance, and behavioral changes associated with autism.
Key microbial influences include:
- Short-chain fatty acids (SCFAs): May influence brain development but can be harmful in excess
- Tryptophan metabolism: Affects serotonin production
- Lipopolysaccharides (LPS): Inflammatory bacterial byproducts that can cross the blood-brain barrier
Natural Strategies to Support Gut-Brain Health in ASD
1. Dietary Interventions
- Implement a gluten-free, casein-free (GFCF) diet if beneficial
- Avoid ultra-processed foods and additives
- Include fiber-rich, whole foods to support microbial diversity
2. Probiotic and Prebiotic Supplementation
- Probiotics such as Lactobacillus plantarum, Bifidobacterium infantis, and Saccharomyces boulardii may support gut balance
- Prebiotics like inulin and FOS can feed beneficial bacteria
3. Address Gut Inflammation and Leaky Gut
- Use nutrients like L-glutamine, zinc carnosine, and omega-3s to support gut lining integrity
4. Consider Targeted Microbiome Testing
- Stool tests can reveal specific imbalances and guide personalized protocols
Final Thoughts
The gut microbiome plays a pivotal role in neurological and behavioral health, particularly in autism spectrum disorder. While no single intervention is a cure, improving gut health through diet, supplementation, and testing can be a powerful part of a holistic support plan. As always, consult with your child’s healthcare provider before making significant changes.
Call to Action: Want to learn more about supporting your child’s gut-brain health? Download our free GFCF recipe guide or book a personalized consultation at OrganiClinic.com.
Autism and Genes, Methylation
Your brain thrives on balance — especially between two key neurotransmitters: glutamate and GABA. Glutamate excites neurons, powering cognition and alertness, while GABA calms the nervous system and promotes relaxation. When this delicate equilibrium shifts toward too much glutamate or too little GABA, symptoms like anxiety, insomnia, irritability, and brain fog can emerge. In this article, we explore science-backed, natural strategies to restore the balance between glutamate and GABA for better mood, focus, and overall brain health.
The Glutamate-GABA Connection
Glutamate is the primary excitatory neurotransmitter in the brain, essential for memory and learning. GABA (gamma-aminobutyric acid) is its inhibitory counterpart, responsible for calming neural activity. In a healthy brain, glutamate and GABA work together in a dynamic push-pull system.
An imbalance — whether from genetics, stress, diet, or environmental toxins — can lead to “excitatory dominance,” where the brain becomes overstimulated. This can contribute to neuroinflammation, mood disorders, and even neurodegenerative conditions over time.
Symptoms of Glutamate-GABA Imbalance
- Anxiety or panic attacks
- Sleep disturbances or insomnia
- Sensory hypersensitivity
- Irritability or mood swings
- Poor focus or cognitive fatigue
Natural Ways to balance glutamate and gaba
1. Magnesium
Magnesium acts as a natural NMDA receptor antagonist, helping to reduce glutamate activity and support GABA production. Magnesium glycinate and threonate are preferred forms for neurological support.
2. L-Theanine
Found in green tea, this amino acid boosts GABA and has a calming effect without sedation. It also modulates glutamate receptors.
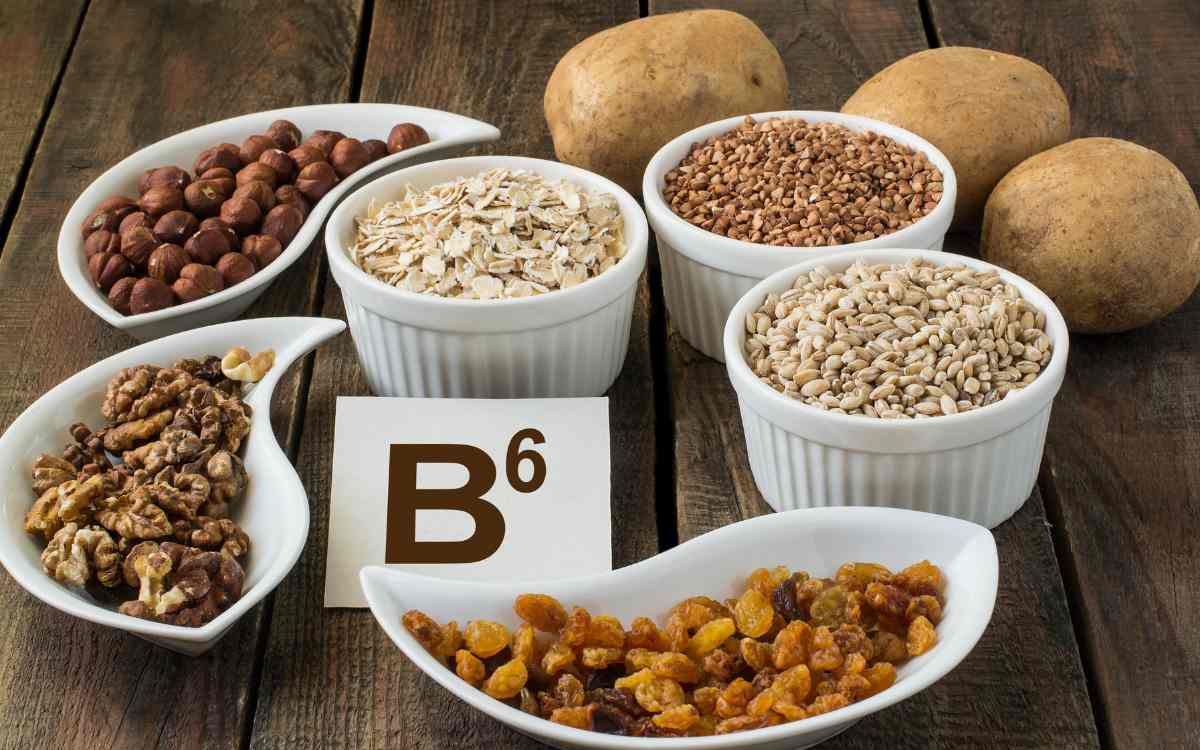
3. Vitamin B6 (P5P)
A crucial cofactor in GABA synthesis, especially for those with genetic variants like GAD1.
4. Taurine
An amino acid that mimics GABA activity and helps stabilize the nervous system.
5. Avoid Excess Glutamate
Reduce dietary intake of glutamate-rich additives like MSG, hydrolyzed protein, and aspartame. These can worsen symptoms in sensitive individuals.
6. Support Gut Health
The gut-brain axis influences neurotransmitter production. Probiotics, prebiotics, and a diverse diet can support GABA-producing bacteria.
7. Balance Blood Sugar
Glucose instability can exacerbate glutamate excess and impair GABA activity. Eat balanced meals with protein, fat, and fiber.
Advanced Considerations
- Genetic SNPs (e.g., GAD1, SLC1A1, COMT) can impact neurotransmitter metabolism. Personalized testing can help guide supplementation.
- Chronic stress depletes GABA. Incorporate stress-reducing practices like breathwork, meditation, or adaptogens (ashwagandha, rhodiola).
Final Thoughts
Balancing glutamate and GABA naturally is a foundational step in supporting brain health, emotional regulation, and mental clarity. Through diet, supplementation, and lifestyle strategies, you can help bring your neurochemistry back into harmony. Always consult with a healthcare provider for individualized guidance.
Call to Action: Want a customized plan to restore neurotransmitter balance? Take our free NeuroBalance Quiz or book a consultation at OrganiClinic.com.

Gut-Brain Axis, Microbiome and Gut health
Development of the Gut Microbiome plays a crucial role in overall health, influencing digestion, immunity, and even mental well-being. The gut microbiome encompasses trillions of microorganisms, including bacteria, viruses, fungi, and protozoa, residing primarily in the human digestive tract. These microorganisms play a vital role in maintaining health by aiding digestion, synthesizing essential nutrients, and modulating immune responses. Research indicates that a well-balanced gut microbiome is integral to several physiological processes, influencing everything from metabolism to mood. Development of the Gut Microbiome
Significance in human health
The gut microbiome significantly impacts overall health, where an imbalance (dysbiosis) can contribute to various conditions, including obesity, diabetes, gastrointestinal disorders, and even mental health issues. Given the microbiome’s complexity, understanding its development throughout an individual’s life offers insights into preventive health strategies and potential therapies for various diseases.
Factors Influencing Development of the Gut Microbiome
Several key factors shape the gut microbiome from infancy through older adulthood:
- Diet: Types of food consumed, such as fiber-rich fruits and vegetables or processed foods, profoundly affect microbial diversity
- Environment: Early exposure to different environments, including natural and urban settings, can influence microbiome composition
- Lifestyle: Physical activity and stress levels play roles in shaping microbiome health and functionality
- Health Status: Pre-existing health conditions, medications (like antibiotics), and overall immune health can alter the microbial landscape
Understanding these factors and their interplay throughout different life stages can inform better dietary and health choices, emphasizing the microbiome’s pivotal role in maintaining overall well-being.
Early Life and Gut Microbiome Development
The initial colonization of the gut microbiome begins at birth, with the mode of delivery being a crucial factor. Infants born via vaginal delivery typically acquire their microbiome from the mother, obtaining beneficial bacteria that lay the foundation for a healthy gut. In contrast, those delivered by cesarean section may have reduced microbial diversity, primarily acquiring bacteria from the surrounding environment and healthcare professionals
Role of Breastfeeding
Breastfeeding further influences gut microbiome development. Human milk contains prebiotics and probiotics that foster the growth of beneficial bacteria, such as Bifidobacterium and Lactobacillus, essential for digestion and immune support. Formula-fed infants might not develop the same microbial diversity, potentially leading to a higher risk of gastrointestinal problems and allergies [8].
Early Dietary Exposures
As infants progress to solid foods around six months, early dietary exposures become critical. Introducing a diverse range of fruits, vegetables, and whole grains can enhance microbial richness. Foods rich in fiber support the growth of good bacteria, whereas processed foods may contribute to dysbiosis [9].
Summary of Influencing Factors
In summary, several factors play a significant role in shaping the gut microbiome in early life:
- Mode of Birth: Vaginal vs. cesarean impacts initial microbial colonization.
- Breastfeeding: Exclusive breastfeeding promotes beneficial bacteria.
- Early Diet: Introduction of diverse solid foods influences microbiome diversity.
Understanding these early-life factors is vital for promoting long-term health and preventing future health issues related to gut health.
Influences of Diet and Environment
Diet and lifestyle choices during childhood and adolescence significantly influence the gut microbiome’s development and overall health. The following elements play crucial roles in shaping the microbial landscape during these formative years:
Processed Foods vs. Whole Foods
- Processed Foods: High in sugars and unhealthy fats, these foods can diminish microbial diversity and promote the growth of harmful bacteria. Frequent consumption may lead to dysbiosis, increasing the risk of metabolic disorders [10].
- Whole Foods: Nutrient-rich, fiber-packed options like fruits, vegetables, whole grains, and legumes foster a diverse microbial community. These foods encourage beneficial bacteria that support digestion and immune function.
Probiotics and Fermented Foods
Incorporating probiotics through foods like yogurt, kefir, and fermented vegetables can positively influence gut health. These live microorganisms enhance microbial diversity and balance the gut environment, especially in children aged between two to six, when the gut is highly adaptable.
Antibiotics Impact
Antibiotic use during childhood, while sometimes necessary, can lead to significant shifts in the gut microbiome. They can eradicate both harmful and beneficial microbes, potentially resulting in long-term health implications. Limiting unnecessary antibiotic prescriptions is vital for maintaining microbiome health.
Environmental Factors
- Pets: Interactions with pets expose children to diverse microbes, enhancing the gut microbiome’s complexity and potentially reducing allergen susceptibility.
- Pollution: Exposure to pollutants can negatively impact microbiome diversity and has been linked to inflammatory conditions and respiratory illnesses.
Understanding these dietary and environmental influences helps promote better health decisions, supporting a resilient gut microbiome throughout life.
Adulthood and the Microbiome
During adulthood, the gut microbiome continues to evolve, influenced by a multitude of factors including stress, diet, and health conditions. This dynamic phase is crucial as individuals face various lifestyle changes that can significantly affect microbial balance.
Impact of Stress
Stress is known to alter gut microbiome composition. Elevated stress levels can lead to increased production of stress hormones, such as cortisol, which may favor the growth of pathogenic bacteria while suppressing beneficial strains. This imbalance, known as dysbiosis, can manifest as gastrointestinal symptoms, mood disorders, and even autoimmune conditions.
Dietary Habits
Diet plays a pivotal role in maintaining a healthy microbiome throughout adulthood. Consuming a diet high in:
- Fiber-rich foods: Whole grains, fruits, and vegetables enhance microbial diversity and promote beneficial bacteria.
- Processed foods: High in sugars and unhealthy fats, these can lead to dysbiosis, contributing to inflammation and metabolic disorders.
Consequently, choices made regarding food not only affect physical health but also your gut health, highlighting the importance of mindful eating.
Lifestyle Choices and Dysbiosis
Adults often encounter lifestyle choices such as alcohol consumption, smoking, and sedentary behavior, all of which can adversely affect the microbiome. For instance, smoking has been linked to decreased microbial diversity, increasing the likelihood of health complications. Conversely, regular physical activity supports a balanced microbiome by fostering beneficial microbial diversity.
Health Conditions and Gut Health
Chronic health conditions like diabetes or obesity can also impact gut well-being. These conditions often induce changes in the gut microbiota, compounding health challenges and making it imperative to monitor and manage gut health proactively.
Understanding these elements allows healthcare professionals to develop strategies for helming healthier lifestyles and mitigating dysbiosis, ultimately improving overall health and wellness.
Aging and the Gut Microbiome
As individuals age, the gut microbiome undergoes significant transformations that can impact health and well-being. These changes often lead to a reduction in microbial diversity, which is crucial for maintaining metabolic and immune functions.
Microbial Diversity and Aging
In older adults, the composition of the gut microbiome tends to shift towards a less diverse ecosystem, primarily characterized by a decline in beneficial bacteria. Key factors contributing to this reduction include:
- Dietary changes: Older adults often consume fewer fiber-rich foods, impacting beneficial bacterial growth.
- Health conditions: Chronic illnesses and medications, particularly antibiotics, can disrupt the microbiome balance, leading to dysbiosis.
- Reduced physical activity: A sedentary lifestyle may also contribute to decreased microbial diversity.
Implications for Overall Health
The implications of these changes are profound, with direct consequences for immune health and disease resistance:
- Immune Function: The gut microbiome plays a crucial role in modulating immune responses. A less diverse microbiome can impair the body’s ability to respond to pathogens effectively, increasing susceptibility to infections.
- Inflammation: Aging-related shifts in the microbiome may promote chronic inflammation, linked to various age-related conditions such as arthritis and cardiovascular disease.
- Metabolic Health: A decline in microbial diversity has also been associated with metabolic disorders, including diabetes and obesity, presenting further health risks for older adults.
Strategies for Improvement
Maintaining a healthy gut microbiome in older adults requires proactive measures. Some effective strategies include:
- Increased fiber intake: Consuming a diet rich in fruits, vegetables, and whole grains promotes the growth of beneficial bacteria.
- Probiotic-rich foods: Incorporating fermented foods like yogurt and kefir can enhance microbial diversity.
- Regular physical activity: Engaging in regular exercise supports a balanced microbiome, improving overall health.
By understanding the dynamics of aging and how they impact the gut microbiome, we can better support the health of older adults, ensuring that they lead vibrant and fulfilling lives.
Conclusion and Future Directions
The development of the gut microbiome throughout a person’s lifetime is a complex journey influenced by numerous factors including diet, environment, lifestyle, and health status. Each stage, from infancy through adulthood and into aging, presents unique challenges and opportunities for microbiome health. Key points of this development underscore the importance of:
- Initial Colonization: Birth mode and breastfeeding can shape the foundational microbial communities.
- Dietary Influences: A shift from whole foods to processed foods can lead to dysbiosis, particularly during childhood and adulthood.
- Aging Effects: With age, microbial diversity tends to decline, which can have detrimental effects on immune function and metabolic health.
Future Research Directions
To unlock the potential of the gut microbiome for health improvements, several areas warrant further investigation:
Microbiome Modulation: Exploring the possibility of intentionally altering the gut microbiome through diet, probiotics, and prebiotics could enhance health outcomes, especially for individuals experiencing dysbiosis.
Therapeutic Interventions: Investigating the efficacy of targeted gut health therapies, including fecal microbiota transplants, could offer new avenues for treating chronic diseases linked to microbial imbalance.
Personalized Nutrition: Understanding microbiome responses to diet can lead to tailored nutritional advice that supports individual microbiome health and overall well-being.
By fostering a deeper understanding of these aspects, future studies can highlight the dynamic relationship between the gut microbiome and human health, paving the way for innovative strategies in disease prevention and management.
References
- https://www.nature.com/articles/nature11234
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/
- https://www.nature.com/articles/s41575-018-0061-6
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7084400/
- https://www.frontiersin.org/articles/10.3389/fmicb.2019.00817/full
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5404430/
- https://www.nature.com/articles/s41591-019-0461-5
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6267732/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5143604/
- https://www.nature.com/articles/nature11234
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6121266/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5369073/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5622713/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/
- https://www.nature.com/articles/nature11400
- https://www.frontiersin.org/articles/10.3389/fmicb.2019.00817/full
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6362717/