
Autism and the GFCF Diet: What Does Science Say and What Do Experiences Show?
Explore the gluten- and casein-free (GFCF) diet in autism—what research says, how it affects the gut–brain axis, and practical tips for families.

Explore the gluten- and casein-free (GFCF) diet in autism—what research says, how it affects the gut–brain axis, and practical tips for families.

Every parent wants to give their child the best possible start in life. While love, safety, and stimulation form the foundation of development, nutrition is one of the most powerful tools for shaping a child’s brain. The foods children eat provide the raw materials for neurons, neurotransmitters, and the networks that enable learning and emotional growth.
This is the heart of Pediatric NeuroNutrition—a field of science that explores how diet influences brain development, behavior, and cognition. For children with unique needs such as autism spectrum disorder (ASD) or ADHD, nutrition can play an even more significant role in supporting brain plasticity, resilience, and daily functioning.
In this article, we’ll examine why early brain development is so unique, which nutrients matter most, how specialized diets like GFCF fit into the picture, and why personalized approaches are becoming the future of child nutrition.
The brain undergoes its fastest growth in the first seven years of life. During this period:
Neurons form connections at astonishing speed—up to one million new connections per second in infancy.
Myelination (the insulating of nerve fibers) progresses, improving communication between brain regions.
Synaptic pruning begins, strengthening the most-used pathways while trimming others.
This phase is marked by brain plasticity—the ability of the brain to adapt and reorganize itself in response to experience and environment. Nutrition directly influences this process by providing:
Structural components (fatty acids for cell membranes).
Co-factors for enzymes (vitamins and minerals).
Energy for signaling and growth.
Poor nutrition during these early years can leave lasting effects on attention, memory, language, and emotional regulation. Conversely, targeted nutrient support can maximize developmental potential.
Role: DHA, an omega-3 fatty acid, is a major structural fat in the brain and retina. It enhances neuronal signaling and reduces inflammation.
Evidence: Higher DHA intake is linked to better language acquisition, visual processing, and emotional regulation.
Sources: Fatty fish (salmon, sardines, mackerel), algae oil supplements.
Role: B vitamins are essential for methylation, neurotransmitter synthesis, and energy metabolism.
Evidence: Deficiencies have been linked to attention difficulties, irritability, and delayed cognitive milestones.
Sources: Whole grains, leafy greens, poultry, eggs, beans.
Role: A critical nutrient for acetylcholine (a neurotransmitter for memory and learning) and phospholipid membranes in neurons.
Evidence: Adequate choline in pregnancy and early childhood supports hippocampal development and long-term memory.
Sources: Eggs, chicken, soybeans, Brussels sprouts.
Iron: Necessary for myelin formation and dopamine metabolism. Deficiency is a leading cause of cognitive delays worldwide.
Zinc: Supports synaptic plasticity and modulates glutamate/GABA balance.
Magnesium: Calms the nervous system and assists in NMDA receptor regulation.
Together, these nutrients form the biological toolkit for brain development—fueling growth, supporting communication, and protecting against oxidative stress.
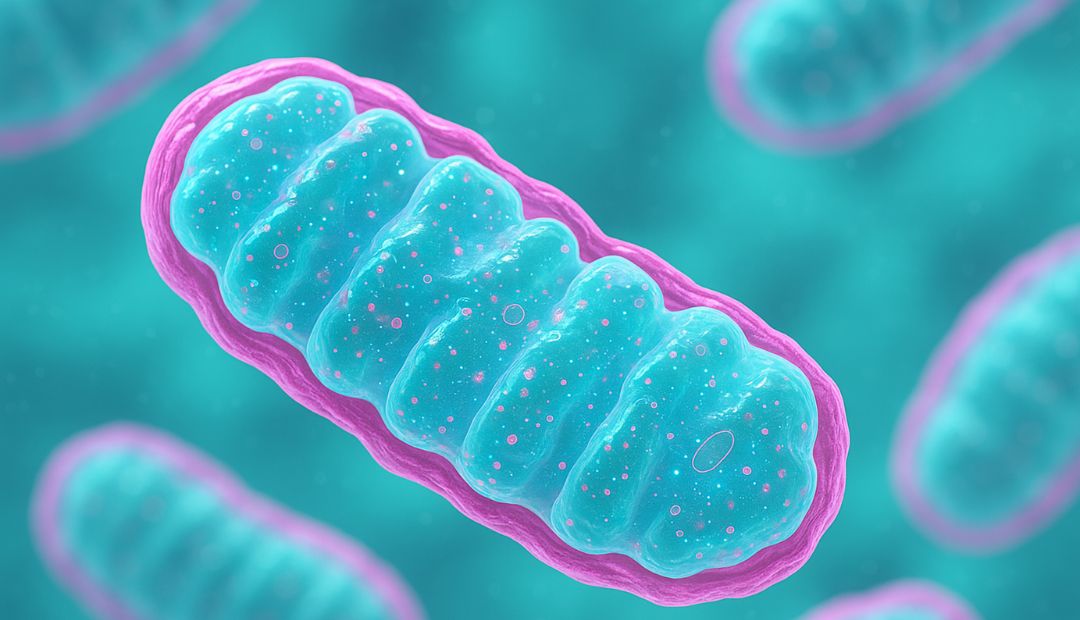
The gluten-free, casein-free (GFCF) diet eliminates gluten (from wheat, barley, rye) and casein (from dairy). It has been widely used in children with autism, ADHD, and sensory processing issues.
Some children with neurodevelopmental conditions have digestive enzyme deficiencies, leading to incomplete breakdown of gluten and casein.
This can produce opioid-like peptides (gluteomorphins, caseomorphins) that affect brain signaling and behavior.
Removing these proteins may reduce brain fog, hyperactivity, and irritability.
While studies show mixed results, many families report:
Improved sleep and mood stability.
Enhanced language skills and social interaction.
By reducing neuroinflammation and abnormal peptide activity, the GFCF diet may create a healthier environment for synaptic plasticity—allowing the brain to rewire more effectively in response to therapies and learning.
Amino acids: Tyrosine and phenylalanine are precursors.
Sources: Poultry, fish, beans, nuts, seeds.
Function: Regulate motivation, attention, and learning.
Amino acid: Tryptophan is the precursor.
Sources: Turkey, eggs, pumpkin seeds, bananas.
Function: Governs mood, sleep, and emotional regulation.
Precursors: Glutamate, vitamin B6, magnesium.
Sources: Fermented foods, spinach, almonds.
Function: Calms overactive neurons and reduces anxiety.
Precursor: Choline.
Sources: Eggs, sunflower seeds, liver.
Function: Memory, attention, and learning capacity.
When children receive adequate building blocks, neurotransmitters remain in balance—helping regulate behavior, focus, and emotional responses.
Many children with autism show altered folate and B12 metabolism. Supplementation with active forms (methylfolate, methyl-B12) has been associated with improved speech, sleep, and social awareness in some cases.
GFCF diet trials reveal reductions in gastrointestinal symptoms and gains in behavior for sensitive children.
Omega-3 supplementation has been linked to better emotional regulation and eye contact.
Iron and zinc deficiencies are common, and correcting them can reduce hyperactivity.
Omega-3 fatty acids may enhance focus and reduce impulsivity.
Diets high in artificial additives have been associated with worsening symptoms in some children.
Better eye contact and responsiveness after nutrient support.
Reduced meltdowns when magnesium and B vitamins are optimized.
Steadier sleep and attention patterns with omega-3 intake.
While not a substitute for therapy or medication, Pediatric NeuroNutrition acts as a complementary strategy to improve outcomes in ASD and ADHD.
Every child’s genetic makeup, gut microbiome, and lifestyle are unique. What benefits one child may not help another—or could even cause sensitivities.
Genetic testing (MTHFR, MTRR, COMT) helps identify nutrient metabolism differences.
Laboratory biomarkers: homocysteine, ferritin, zinc, vitamin D, fatty acid profiles.
Dietary tracking: Observing food logs and behavior journals for patterns.
Start with a nutrient-dense foundation: whole foods, colorful vegetables, lean proteins, healthy fats.
Address deficiencies first: iron, vitamin D, zinc are common.
Introduce changes gradually: one supplement or diet shift at a time.
Work with professionals: pediatricians, dietitians, or integrative practitioners experienced in neurodevelopment.
Personalized nutrition means meeting the child where they are, supporting their unique biology, and adjusting over time as they grow.
The first seven years of life represent a critical window for brain development shaped by nutrition.
Key nutrients—DHA, B vitamins, choline, and minerals—provide the building blocks for neurons and neurotransmitters.
The GFCF diet may reduce neuroinflammation and support brain plasticity in some children.
Neurotransmitter balance depends on dietary precursors like tryptophan, tyrosine, and choline.
Clinical experience shows nutrition can improve behavior, sleep, and learning in autism and ADHD.
Personalized nutrition is the most effective approach, tailoring diets and supplements to each child’s needs.
1. What is Pediatric NeuroNutrition?
It’s the science of using diet and nutrients to support brain development, behavior, and learning in children.
2. Which nutrient is most important for brain development?
No single nutrient is enough. DHA, B vitamins, choline, and minerals all work together to build and support the brain.
3. Does the GFCF diet help every child with autism?
No. Some children benefit greatly, others show little change. It should be tried under professional supervision.
4. How soon can parents see results from nutrition changes?
Some notice improvements within weeks; for others, it may take months of consistent support.
5. Can diet replace medication in ADHD or autism?
Diet is not a replacement but can significantly complement medical and therapeutic care.
6. Are supplements safe for children?
When guided by a healthcare provider, supplements can be safe and effective. Avoid self-prescribing high doses.
7. What’s the best first step for parents?
Focus on a nutrient-rich diet, then consider testing and professional guidance for personalized support.
Pediatric NeuroNutrition offers a roadmap for parents who want to support their child’s brain development through food and nutrients. By understanding the critical windows of brain growth, the roles of DHA, B vitamins, choline, and minerals, and the potential of specialized diets like GFCF, families can make empowered choices.
While autism and ADHD present unique challenges, nutrition provides a foundation for improved brain plasticity, better behavior, and stronger learning potential. Personalized approaches ensure that each child’s diet matches their genetics, environment, and developmental stage.
Nutrition cannot rewrite every challenge, but it can strengthen the brain’s capacity to adapt, learn, and thrive—helping children build brighter futures, one meal at a time.

Discover how methylation and gene mutations like MTHFR influence autism, brain development, and child health, plus practical support strategies.

Discover how Pediatric NeuroNutrition supports children with autism through methylation balance and nutrigenomics for better health, behavior, and learning.



Does your day start with a rushed coffee, spike around school‑run time, dip at 3 p.m., and limp toward bedtime with nothing left for yourself? You are not alone. For many moms and health‑conscious women, fatigue, cravings, and mood swings feel like part of the job description. These symptoms often hide a deeper biological story—one where your body’s ability to methylate and to balance blood sugar dance together in a delicate rhythm.
Methylation is a fundamental biochemical process that transfers a methyl group (one carbon and three hydrogens—CH₃) onto DNA, proteins, neurotransmitters, and hormones. Think of it as the body’s “on/off” switch for gene expression, detoxification, hormone metabolism, and more. Without efficient methylation, downstream systems—including glucose regulation—struggle.
Recent studies show DNA‑methylation patterns correlate with insulin resistance and Type 2 diabetes risk, independent of weight or family history. One cross‑ancestry analysis found specific CpG sites within the TXNIP gene consistently associated with insulin resistance. (pmc.ncbi.nlm.nih.gov) Another 2024 systematic review concluded that aberrant DNA methylation is both a marker and potential driver of Type 2 diabetes progression. (clinicalepigeneticsjournal.biomedcentral.com) In simpler terms: how well you add those tiny CH₃ tags can nudge your blood sugar higher or lower.
Methylation lives inside the one‑carbon cycle, powered by nutrients like folate, vitamins B‑12, B‑6, riboflavin, choline, betaine, and the amino acid methionine. Dietary folate converts to 5‑MTHF, donates a methyl group to homocysteine, forming S‑adenosyl‑methionine (SAMe)—the body’s universal methyl donor.
Key checkpoints:
These pathways collectively influence hepatic glucose output, pancreatic β‑cell health, and insulin signaling.
Some women carry single‑nucleotide polymorphisms (SNPs) that slow these enzymes. A 2024 Chinese study linked MTHFR C677T and A1298C variants with a 2.24‑fold higher Type 2 diabetes risk. (pubmed.ncbi.nlm.nih.gov) Another meta‑analysis found the T allele increases odds of gestational diabetes, a key concern for future moms. (frontiersin.org) Translation: your genes may demand extra methyl‑support.
Pregnancy, postpartum, oral contraceptives, and perimenopause all shift estrogen and progesterone, increasing need for folate, B‑12, and choline just as growing babies or hormonal swings intensify blood‑sugar fluctuations. Elevated estrogen can heighten insulin sensitivity; progesterone can push the other way. Efficient methylation helps smooth this seesaw.
Conventional panels often miss sub‑optimal methylation. Consider adding:
Carbohydrates → glucose in bloodstream → insulin released → GLUT4 transporters shuttle glucose into muscle & fat → stored as glycogen or triglycerides. Efficient methylation supports this by modulating hepatic enzymes and reducing oxidative stress that can blunt insulin receptors.
| Marker | Conventional Upper Limit | Functional Optimal |
|---|---|---|
| Fasting Glucose | 99 mg/dL | 75–90 mg/dL |
| HbA1c | 5.6 % | 4.9–5.2 % |
| Post‑Meal (1 h) | <180 mg/dL | <140 mg/dL |
| CGM Daily Variability (SD) | — | <20 mg/dL |
SAMe donates methyl groups to enzymes regulating PEPCK and G6Pase, gatekeepers of gluconeogenesis. Low SAMe → overactive glucose production at night → elevated fasting glucose.
Chronic stress boosts cortisol, which raises blood sugar. COMT (catechol‑O‑methyltransferase) uses methyl groups to break down catecholamines (adrenaline, noradrenaline). Insufficient methylation → slower clearance → prolonged stress response → higher glucose.
High homocysteine stiffens blood vessels and reduces nitric‑oxide‑mediated vasodilation, impairing glucose delivery to muscle. (frontiersin.org) Even if insulin is normal, transport is slowed—raising circulating glucose.
Background: Postpartum weight plateau, afternoon crashes, family history of Type 2 diabetes.
Initial Labs:
Intervention (12 weeks):
Outcome:
| Food Group | Purpose | Easy Swaps |
| Folate‑Rich Greens | Provide 5‑MTHF | Spinach smoothie > cereal |
| Lean Protein | Slows glucose rise; supplies methionine | Greek yogurt parfait > muffin |
| Resistant Starch | Feeds gut microbes → better insulin sensitivity | Cooled quinoa salad > white rice |
| Healthy Fats | Sustain satiety, support cell membranes | Avocado slices > low‑fat dressing |
| Colorful Polyphenols | Reduce oxidative stress on β‑cells | Berries > candy |
| Need | Key Nutrient | Dose Range |
| Folate cycle | 5‑MTHF or folinic acid | 400–1,000 µg/day |
| B‑12 support | Methyl‑ or hydroxocobalamin | 500–2,000 µg/day sublingual |
| Homocysteine clearance | Vitamin B‑6 (P5P) | 25–50 mg/day |
| Betaine support | Trimethylglycine (TMG) | 500–1,000 mg with meals |
| Insulin sensitivity | Magnesium glycinate | 200–400 mg at night |
| PCOS/Cravings | Myo‑inositol | 2–4 g divided |
Red flags include fasting glucose >100 mg/dL, HbA1c >5.6 %, or homocysteine >9 µmol/L despite diet.
Your body’s methylation rhythm is the unseen conductor of blood‑sugar harmony. Start tuning it today—begin with one folate‑rich meal, one mindful breath, one step toward balanced living.
©2025 Organiclinic. This content is for educational purposes and does not substitute individualized medical advice.