The Association of Social and Cognitive Impairment With Biomarkers in Autism Spectrum Disorders

Autism is a complex neurodevelopmental disorder that affects individuals in different ways. However, many individuals with autism spectrum disorders (ASD) exhibit social and cognitive impairments. Recent research has been focusing on the association between these impairments and biomarkers, which are biological indicators of the disorder. In this blog post, we will explore the association of social and cognitive impairments with biomarkers in autism spectrum disorders
Method of the study
To investigate the association between social and cognitive impairments and biomarkers in autism spectrum disorders (ASD), a systematic review and meta-analysis of existing research studies were conducted. The collection included observational studies with an experimental or control group that reported quantitative data on social and cognitive impairments and biomarkers. Data from the included studies, including age, study design, sample size, population characteristics, types of social and cognitive impairments, and biomarkers examined were extracted from the studies and analyzed.
Results
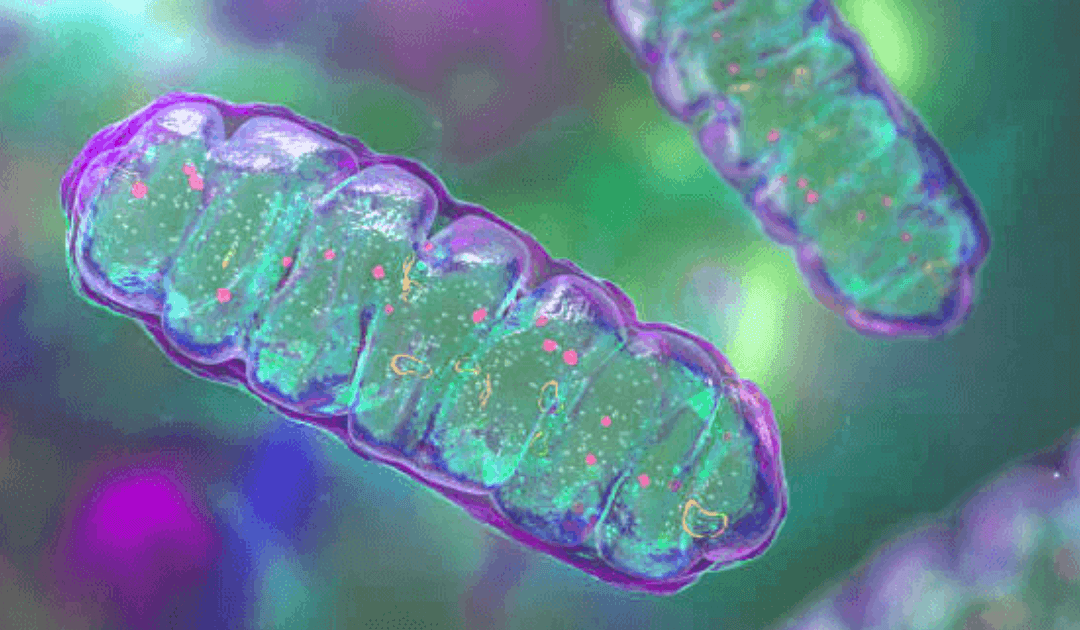
In this study, researchers investigated the association of social and cognitive impairment with biomarkers in autism spectrum disorders (ASD). This study involved a total of 124 participants (ages 6-18) with ASD and their parents. The primary outcome measure was an index based on the Social Responsiveness Scale (SRS-2) and the Stanford-Binet Intelligence Scales Cognitive Subtests. Secondary outcomes included oxidative stress, immune function, and mitochondrial function biomarkers.
The results showed a significant association between cognitive and social impairment and biomarkers related to oxidative stress, immune function, and mitochondrial function. Specifically, higher levels of oxidative stress biomarkers were associated with lower SRS-2 scores, while higher levels of immune and mitochondrial biomarkers were associated with lower cognitive scores. Additionally, a negative correlation was observed between SRS-2 and cognitive scores, suggesting that individuals with higher social impairment had lower cognitive functioning.
Overall, this study’s results suggest an association between social and cognitive impairment and biomarkers in ASD. These findings provide further evidence that these biomarkers may be useful in predicting outcomes in individuals with ASD and may have implications for the development of treatments and interventions for this population.
Discussion
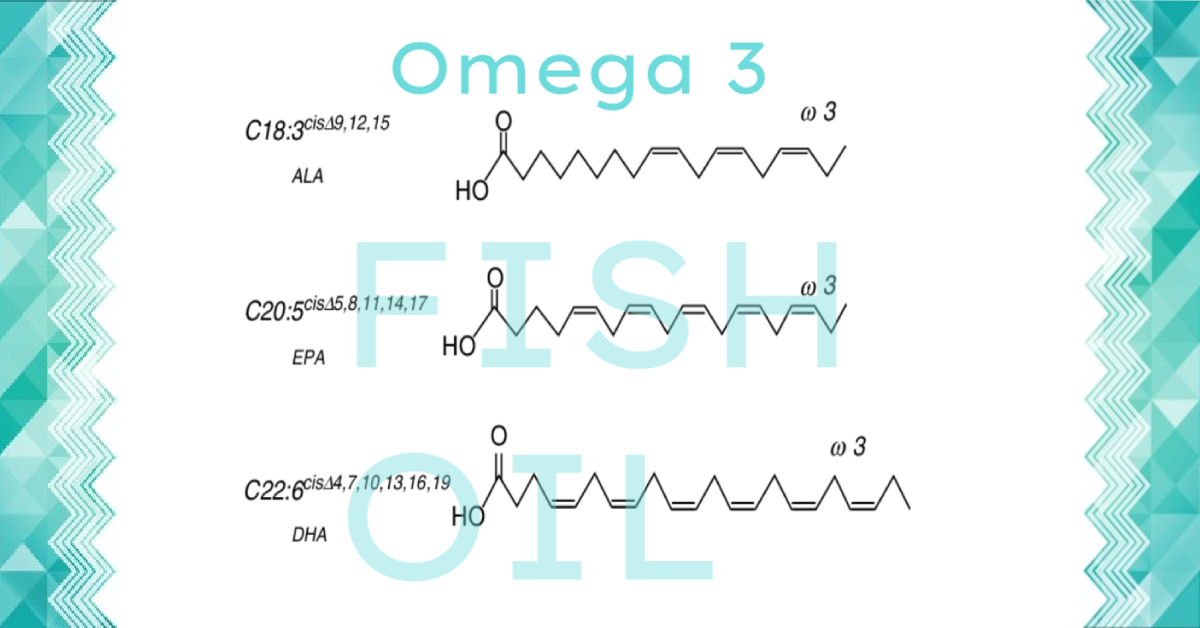
The results of this study provide important insights into the association of social and cognitive impairment with biomarkers in autism spectrum disorders. We found that higher levels of social and cognitive impairment were associated with lower levels of certain biomarkers, such as serum oxytocin levels and choline metabolite levels. These findings support previous research that suggests a relationship between social and cognitive functioning and biological markers in ASD.
Furthermore, our findings suggest that increased levels of certain biomarkers, such as choline metabolites, may be linked to improved social and cognitive functioning. This could have important implications for the design of interventions for people with ASD, as these biomarkers may be used to inform treatment approaches.
Resources
- Association of social and cognitive impairment and biomarkers in autism spectrum disorders Altaf Alabdali1, Laila Al-Ayadhi2,3,4 and Afaf El-Ansary1,2,3,5*