Histamine intolerance or MCAS?
Histamine intolerance or MCAS (Mast Cell Activation Syndrome.) There is not much difference between the symptoms of these two health issues. In this article, we discuss the details related to the difference.
Difference between Histamine Intolerance and Mast Cell Activation Syndrome
The main difference between MCAS and histamine intolerance is that in MCAS, mast cells are not working correctly and release excessive chemical mediators. In contrast, histamine intolerance is a condition in which dietary histamine accumulates in the body because the body cannot break it down. (1)
Histamine intolerance is a so-called subset of MCAS. If you have discovered you have histamine intolerance, you need to test MCAS. (2)
What are mast cells?
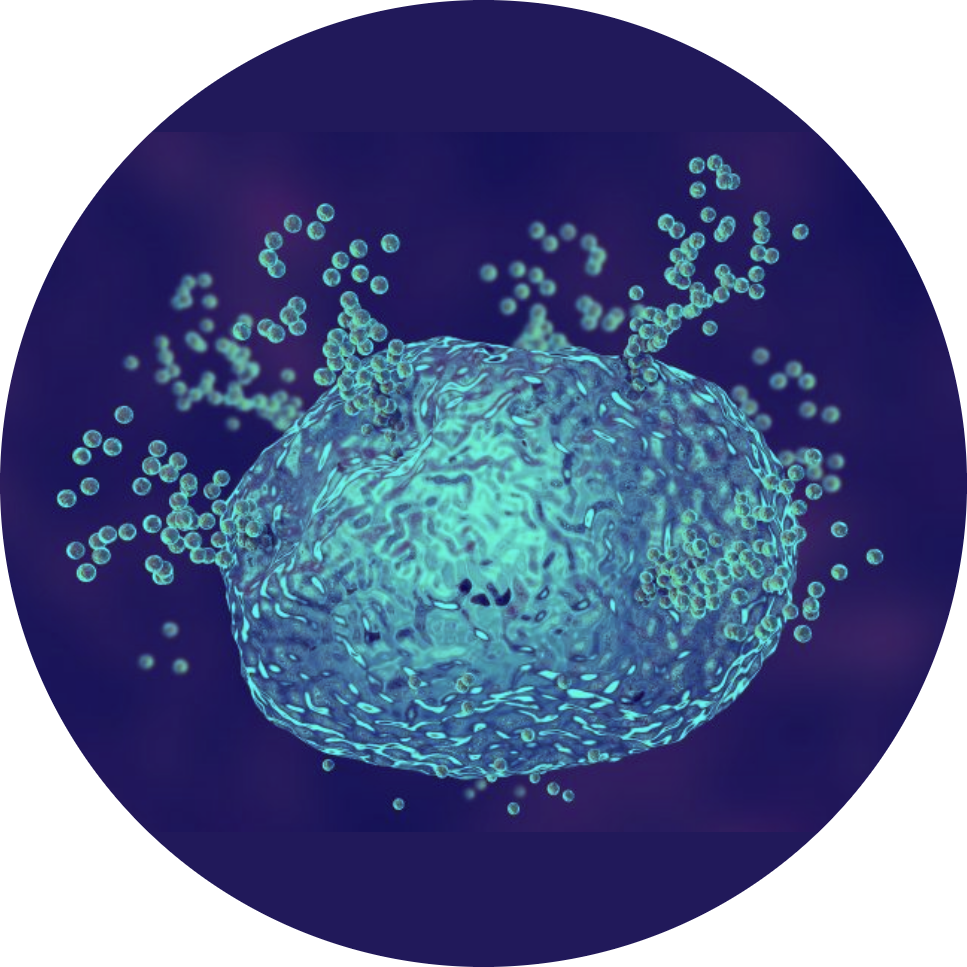
Mast cells are particularly found in tissues that are in close contact with the environment such as skin, airways, and gastrointestinal tract but are found in most tissues throughout the body.
Mast cells are types of white blood cells that release up to 200 signaling chemicals, ie. mast cell mediators into the body as part of an immune system as a defense response against foreign invaders (parasites, fungi, bacteria, or viruses), allergens and environmental toxins.
Mast cell mediators include histamine, proteases, leukotrienes, prostaglandins, chemokines, and cytokines, and their job is to signal and guide other cells, tissues, and organs to respond to the hostile invaders, therefore mast cells are protecting us from infection, heal wounds, create new blood cells, and develop immune tolerance.
However, if these cells are dysfunctional or overactive, they can cause serious issues. (3) In case of MCAS the mast cells secrete too much mediators, not just histamine, though, histamine is still a major component.
What is Mast Cell Activation Syndrome?
Mast cell activation syndrome (MCAS) is an immunological condition where mast cells inappropriately release excessive chemical mediators. (4) In most cases, this condition is mild, however, it can exacerbate due to stressful life events.
MCAS symptoms
The symptoms of MCAS are the same as those of histamine intolerance. The difference between these two health problems may be that while histamine intolerance is caused by some kind of inflammation and methylation disorder or/or DAO enzyme deficiency, which may improve after the cause is removed, in the case of MCAS, the mast cells are too sensitive to triggers and often inexplicably the patient produces symptoms for no reason, and this state of health can hardly be reversed, it can only be maintained.
The most common symptoms of MCAS include:
- The trouble with allergies and asthma
- Overreaction to insect bites, bee stings, and chemical intolerances
- Facial and chest flushing skin rashes including hives and angioedema
- Itchiness and a burning feeling
- Brain fog and headaches
- Poor wound healing and easy bruising
Symptoms in bulk:
Red eyes, irritated eyes, dry eyes, burning eyes, vision problems and conjunctivitis, nasal congestion, sinusitis, runny nose, laryngitis and intranasal wounds, tinnitus, clogged, acne, acne wounds, itchy throat, itchy throat difficulty swallowing, hives, skin flushing, itching, skin rashes, flushing, bruising easily , angioedemareddish or pale complexion, cherry angiomata (skin growths), patchy red rashes, red face in the morning, cuts that won’t heal, fungal skin infections, fainting, fainting upon standing, increased pulse rate (tachycardia), palpitations, spikes and drops in blood pressure, high pulse or temperature, high triglycerides, lightheadedness, dizziness, hot flashes, wheezing, asthma, shortness of breath, difficulty breathing deep, abdominal pain, epigastric tenderness, nausea, vomiting, diarrhea and/or constipation, abdominal cramping, bloating,
GERD/acid reflux, high colesterol, high bilirubin, elevated liver enzymes, numbness and tingling in the hands and feet, headaches, migraines tics, tremors, brain fog, memory loss, poor concentration, difficulty finding words, muscle pain, fibromyalgia, muscle weakness, blood clots, deep vein thrombosis, increased bruising, heavy menstrual bleeding, bleeding nose, anemia, increased white blood cell count, platelets, decreased white blood cell counts, decreased neutrophils, decreased lymphocytes, decreased platelets, excesses of IgA, IgG, IgM, IgE, increased MCV, anxiety, panic, depression, decreased attention span, attention deficit/hyperactivity disorder (ADHD), forgetfulness, and insomnia, anaphylaxis.
Possible causes
The exact cause of mast cell activation syndrome is unknown. It is sometimes called an idiopathic condition because it is hard to determine the exact thing that triggers mast cell overactivation. (6)
This condition can be present if the mast cells are abnormal but in secondary MCAS, the mast cells themselves are normal, but they become abnormally activated by an external stimulus. People with secondary MCAS have triggers that provoke an exaggerated immune response. MCAS actually is a multisystem condition and the main suspected cause in most cases is some form of inflammation. If you have been diagnosed with any of the following conditions, probably MCAS can also be detected. Health issues may include, but are not limited to the following (7):
Chronic Inflammatory Response Syndrome (CIRS)
Irritable bowel syndrome
Intestinal dysbiosis
SIBO
Obesity, Diabetes
Toxins
Asthma and allergies
Autoimmune diseases (lupus, rheumatoid arthritis and Hashimoto’s disease)
Candida overgrowth
Celiac disease
Parasitic infections
Skin diseases such as eczema and psoriasis
Food intolerance and allergies
Gastroesophageal Reflux (GERD)
Infertility and endometriosis
Health conditions that can aggravate MCAS:
Chronic inflammatory response syndrome (CIRS),
Poor methylation due to genetic MTHFR defects (leading to low SAMe levels that degrade histamine intracellularly),
Histamine N-methyltransferase HNMT enzyme deficiency.
Lack of an enzyme based on intestinal diamine oxidase (DAO) that breaks down histamine of food. (8,9)
Diagnosis of mast cell activation syndrome (11)
First of all the proper diagnosis of MCAS requires the presence of several symptoms from the list above. In addition, other disorders should be ruled out by a functional medicine professional.
When symptoms listed above affecting at least 2 organs are present and they are chronic and are found not to be caused by another health condition, the presence of MCAS is suspected.
The second necessary criteria is the examination of serum tryptase levels, i.e., if the tryptase level rises above a threshold within a narrow (usually one to two hours) time interval after a symptomatic episode. According to the consensus serum tryptase levels that are at least 20% above baseline serum tryptase levels, plus 2 ng / ml, after the onset of symptoms, meets the second criterion of mast cell activation syndrome.
For example, if a patient had a basal (baseline level, at least 24 hours after a reaction) serum tryptase level of 8 ng/ml, a 20% rise, plus 2 ng/ml, would be 11.6 ng/ml. To meet the above criterion for serum tryptase, the patient would need a post-reaction serum tryptase level above 11.6 ng/ml. The calculation would be conducted as follows:
(8 ng/ml x 1.2) + 2 ng/ml = 11.6 ng/ml
If tryptase level does not rise sufficiently to meet the growth required for the co-criterion, other mediator tests may be sufficient. Examples include elevated urinary n-methylhistamine, prostaglandin D 2 or its metabolite, 11β-prostaglandin F 2α (24-hour urine test for any of the three).
Finally, the third co-criterion requires a response to drugs that inhibit the action of histamine and to drugs that inhibit other mediators produced by mast cells or inhibit the release of mast cell mediators. You can read about this in moredetails in the “Balance your histamine release protocol”.
Resources
- m B-R, SeoH-S, Ku J-M, et al. Silibinininhibits the production of pro-inflammatory cytokines through inhibition of NF-κB signaling pathway in HMC-1 human mast-cells. Inflammation. Research. 2013;62(11):941-950. doi:10.1007/s00011-013-0640-1.
- ChapowalA. PetasitesStudy Group. Randomisedcontrolled trial of butterbur and cetirizine for treating seasonal allergic rhinitis. BMJ 2002;324:144-6.
- Hayes, N. A. and Foreman, J. C. The activity of compounds extracted from feverfew on histamine release from rat mast-cells. J Pharm Pharmacol1987;39(6):466-470
- Hsieh et al. Baicalein inhibits IL-1ß- and TNF-a-induced inflammatory cytokine production from human mast-cells via regulation of the NF-?B pathway. ClinMolAllergy. 5: 5. 2007.
- TheoharidesTC, Patra P, Boucher W, et al. Chondroitin sulphateinhibits connective tissue mast-cells. British Journal of Pharmacology. 2000;131(6):1039-1049. doi:10.1038/ sj.bjp.0703672.
- Ro JY, Lee BC, Kim JY, et al. Inhibitory mechanism of aloe single component (alprogen) on mediator release in guinea pig lung mast-cells activated with specific antigenantibodyreactions. J PharmacolExpTher. 2000;292:114–121. 73.
- https://www.ncbi.nlm.nih.gov/pubmed/24477254
- https://www.ncbi.nlm.nih.gov/pubmed/28458279
- https://www.ncbi.nlm.nih.gov/pubmed/9421440
- https://www.ncbi.nlm.nih.gov/pubmed/10344773
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4315779/

