Histamine intolerance literally does not exist. Intolerance does exist to other externally administered substances, e.g. fructose, lactose. Histamine is constantly produced and broken down in the body, histamine taken from the outside is not normally a problem, on the contrary, it has many benefits.
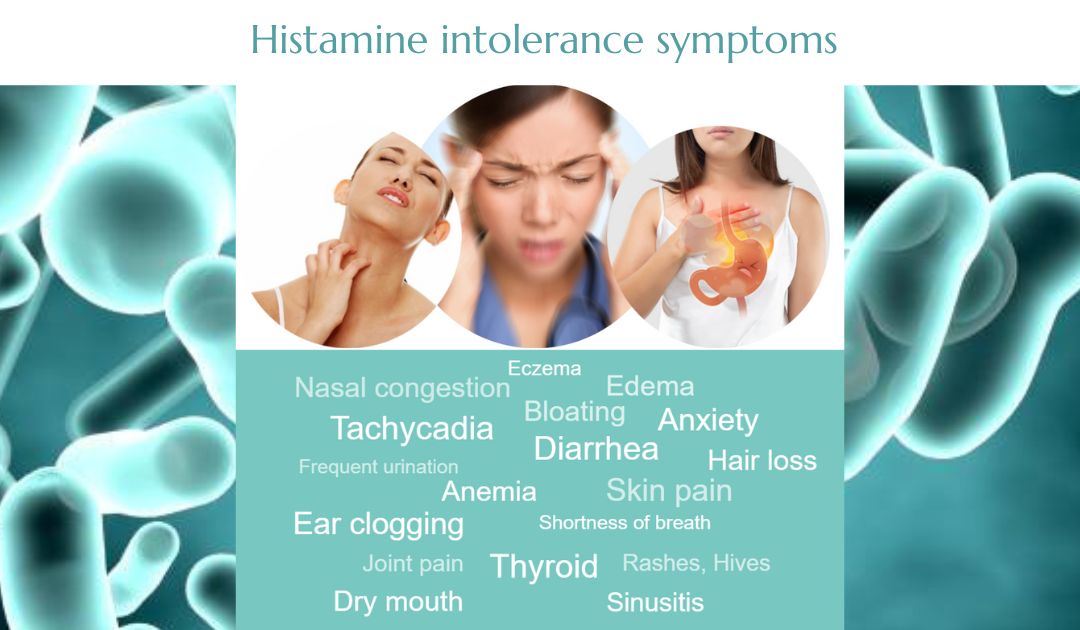
Histamine intolerance symptoms and causes
Histamine intolerance symptoms are extremely varied. First, before diving into this topic, you need to understand what histamine intolerance is.
Although histamine intolerance does not exist in this context, we will use this term to describe this complex phenomenon because it is prevalent in the public consciousness in this name.
Understanding the role of histamine in our body can help us understand the processes behind histamine intolerance. Histamine is a tissue hormone produced by the enzyme histidine decarboxylase and vitamin B6 from the amino acid histidine. This process takes place in many plant and animal organisms. Histamine, an amazingly versatile and vital hormone widely used in the living world, has an effect on life or cells from the first moment of our lives. Histamine plays a neurotransmitter role in our body, both in the central and peripheral nervous systems.
In our body, histamine acts on cells mainly at 4 receptor types [1].
H1 receptors:
It causes contraction of the intestinal, bronchial and uterine smooth muscle tissues
It constricts the wall of small veins, dilates the wall of the arteries
Nerve cells: Pain, itching
Central nervous system: Increased alertness
Ovaries: Estrogen release
Uterus: Supports ovarian implantation
H2 receptors:
Stimulation of gastric secretion
Increasing heart rate, heart rate
Increasing muscle tension
Increased immune defense
H3 receptors:
Like H1 receptors, causes alertness and increased concentration
Inhibition of serotonin, GABA, and acetylcholine release in the peripheral nervous system,
Regulation of hunger and thirst in the central nervous system
H4 receptors:
Enhancement of cellular immune defense
Increasing the inflammatory readiness of skin cells
The condition called histamine intolerance
The condition called histamine intolerance (also known as histaminosis) involves complex, different organ systems with colorful, very different individual conditions. Symptoms, despite their color, show characteristic patterns. Symptoms can be triggered by certain foods, medications, chemicals, and the intensification of symptoms that later affect psychological stress.
Histamine intolerance is not a diagnosis but a concept/description to summarize symptoms. Stakeholders often respond to certain foods that either contain histamine, block certain histamine-degrading pathways, or even bloat (FODMAP fibers).
The Background
The background of the symptom formation called histamine intolerance is, in many cases, the excessive activity of mast cells, in particular mast cells. There is often an inflamed intestinal wall and a lack of micronutrients. Symptoms may also be caused by deficiencies in the two enzymatic pathways that degrade histamine, such as a lack of the enzyme diamine oxidase (DAO) and the lack of micronutrients required for the production of the DAO enzyme (vitamin C, vitamin B6, copper, manganese) and also the lack of micronutrients required for the enzyme (HNMT) (B12, folic acid, magnesium, zinc). Decreased enzyme activity can also be caused by genetic factors, which can predispose some people to symptoms. In the case of a proper supply of nutrients, they do not appear because the body usually maintains several pathways to perform a given function, so there are 2 enzyme systems available for the breakdown of histamine.
The Whithrawal
Withdrawal of symptomatic foods from the diet is, at most short-term relief. A true, lasting solution to histamine intolerance is achieved through a complex, personalized approach. This includes the regeneration of the digestive system, the targeted support of biochemical pathways for the breakdown of histamine, and to the regulation of the hormonal effects of overactivity of histamine-producing immune cells and, if necessary, to detect and counteract underlying chronic infections.
The list of Histamine intolerance symptoms
Individual sensitivity is very different. Some patients do not tolerate any amount of histamine in their food, while others are sensitive only to foods with the highest histamine content [2]. Some people only respond to certain foods containing histamine, not others, or they may only respond to foods that cause specific bloating. In the most severe cases, patients do not tolerate the smallest amount of histamine.
Gastrointestinal symptoms:
Stomach cramps, IBS
Nausea, vomiting
Puffiness
Reflux, feeling acidified
Diarrhea, less often constipation
Mucus production
Crohn’s disease is also common in patients
Dermatological problems:
Hives, eczema [3], neurodermis
Local edema (e.g., around the mouth)
Cardiovascular symptoms:
Fast heartbeat, extrasystoles
Blood pressure drop, sometimes high or fluctuating pressure
Dizziness, fainting
Edema
Psychiatric symptoms:
Flushing, anxiety, panic attack
Strange feelings, feeling of emptiness, depersonalization, derealization
Allergological and immunological symptoms:
Sore throat, cough, frequent sore throat
Clogged nose, runny nose, nasal polyps, chronic sinusitis
Asthma bronchiale (exogenous, ie. caused by pollen, animal hair, mold, or endogenous, ie. without known cause, but after consumption of wine, cheese, or tuna)
Some cases of drug allergy
Histamine entering the bloodstream can also cause anaphylactic shock
Gynecological symptoms:
Menstrual cramps, cramps
Other:
Headache, migraine
Swelling of the lower eyelid
What is in the background?
The following partly mutually reinforcing problems may play a role in the development of histamine intolerance:
1.
Poor gastric function, low gastric acid, and digestive enzyme deficiencies: Due to reduced efficiency of protein digestion, undigested proteins are broken down in the gut by pathogenic bacteria, some of which produce histamine directly.
2.
The entire digestive system, stomach, pancreas, etc., innervation of the parasympathetic nervous system, so it occurs by the Vagus nerve, weak gastric function, and digestive enzyme deficiency may be due to weaker gastrointestinal innervation due to chronic stress.
3.
The pathogens of Lyme disease, Borrelia, can also damage the Vagus nerve, which is why Lyme disease often appears with gastrointestinal symptoms, enzyme deficiencies, and histamine intolerance.
4.
Strong symptom formation often occurs after antibiotic treatments. The destruction of beneficial bacteria and the overthrow of the intestinal flora allow room for the growth of histamine-producing bacteria. In addition, repeated or higher doses of antibiotics may impair mitochondrial function, leading to a reduction in the production of steroid hormones, mast cell activation, and histamine intolerance in addition to general tissue energy deprivation.
5.
Inadequate diet, micronutrient deficiency: The enzymatic degradation pathways of histamine are highly demanding of micronutrients and vitamins.
6.
Immunological problems: Chronic infections are often present in the background of increased activity of histamine-producing mast cells, e.g., Lyme disease, but dental foci can also occur.
7.
Endocrine problems: Higher levels of estrogen and progesterone resp. Lack of cortisol triggers increased activity of histamine-releasing mast cells.
8.
In the case of vitamin B12, folic acid, and magnesium deficiencies, the breakdown of histamine is inadequate;
9.
In vitamin D deficiency, mast cells release more histamine.
10.
Mitochondrial dysfunction: Chronic infections, micronutrients, and vitamin deficiencies are also common, and toxic metal loads, sometimes the toxic effects of drugs or other intoxications may play a role.
How to help histamine intolerance?
When solving histamine intolerance, it is worth distinguishing between short and long-term solutions. Avoid foods that contain or release histamine and cause common symptoms in the short term for about 3-4 weeks. Complicated lists and tables of differently classified foods in terms of histamine can be found here: SIGHI list.
In the longer term, a strategy is needed that includes micronutrient replenishment and, thus, the gradual return of foods that contain or release histamine. Foods that cause individual sensitivity should be reloaded only slowly, in parallel with the regeneration of the body, always taking into account the current individual sensitivity.
Foods containing histamine have many positive effects, some of which are high in micronutrients. Dietary histamine also increases gastric acid levels, which improves protein digestion, kills pathogen-producing bacteria that also produce histamine, and helps utilize vitamin B12.
The problem and the biological background of histamine intolerance are often confused in practice with mast cell activation syndrome (MCAS), so the solutions are similar. For more information on specific protocols and adjuvants, see the MCAS article.
Histamine intolerance can be made asymptomatic and stable even under severe physical or mental strain: Targeted dietary, lifestyle, and nutritional supplementation protocols, partly based on laboratory results, and digestive regeneration improve the body’s vitamin and micronutrient levels. Although the regulation of the functions of the digestive system and the intestinal flora, in most cases, a stable, drug-free state can be achieved.
Other contexts
The symptoms associated with histamine metabolism are not always clearly distinguishable; in some cases, histamine intolerance, mast cell activation disease (MCAD), or mast cell activation syndrome (MCAS). In practice, it is rare to see cases of “pure” histamine intolerance; in most patients, mixed symptoms are reported.
Mastocytosis is not mast cell activation syndrome; the two concepts are often confused. During mastocytosis, more significant amounts of mast cells accumulate in the skin or some organs. The cause is unknown to science. Correlations with IgE-mediated allergies, mental and psychiatric illness, and low vitamin D levels have also been found [5].