Leaky Gut
Symptoms and causes
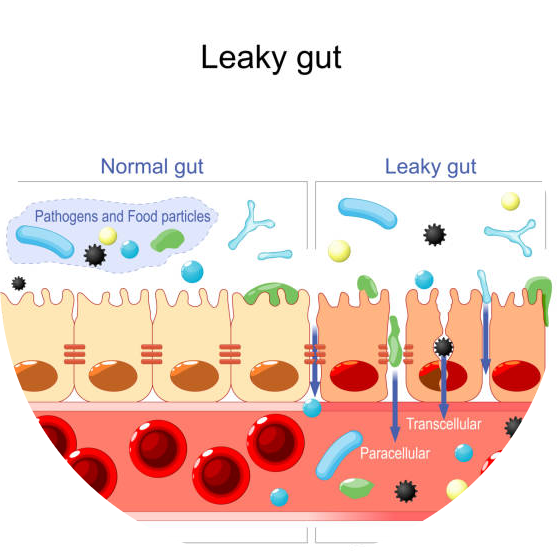
Normally, the bowel does not leak. However, if there is a problem with the intestinal tract, the intestinal wall can also penetrate, leading to inflammation.
On the one hand, the intestines must be sufficiently permeable to absorb nutrients and fluids. Still, they also need a defense mechanism that retains harmful substances and pathogens. The nutrients come from the outside world, i.e., many microorganisms, chemicals, and toxins are ingested daily through food and drink, which enter the body through the intestinal tract.
Formation of Leaky Gut Syndrome
The gut as a defense system
The first stop of this defense system is the barrier, i.e. the gut flora, or as it is now called: the microbiome.
The beneficial bacteria in the gut flora are capable of:
- To destroy pathogens
- “Filters out” various toxins, carcinogens,
- to produce substances that nourish the cells of the intestinal wall,
- they also take part in mucus production, which involves the inner surface of the gut,
- They make B vitamins, folic acid, short-chain fatty acids,
- “Inform” the immune system of the presence of pathogens and harmful substances.
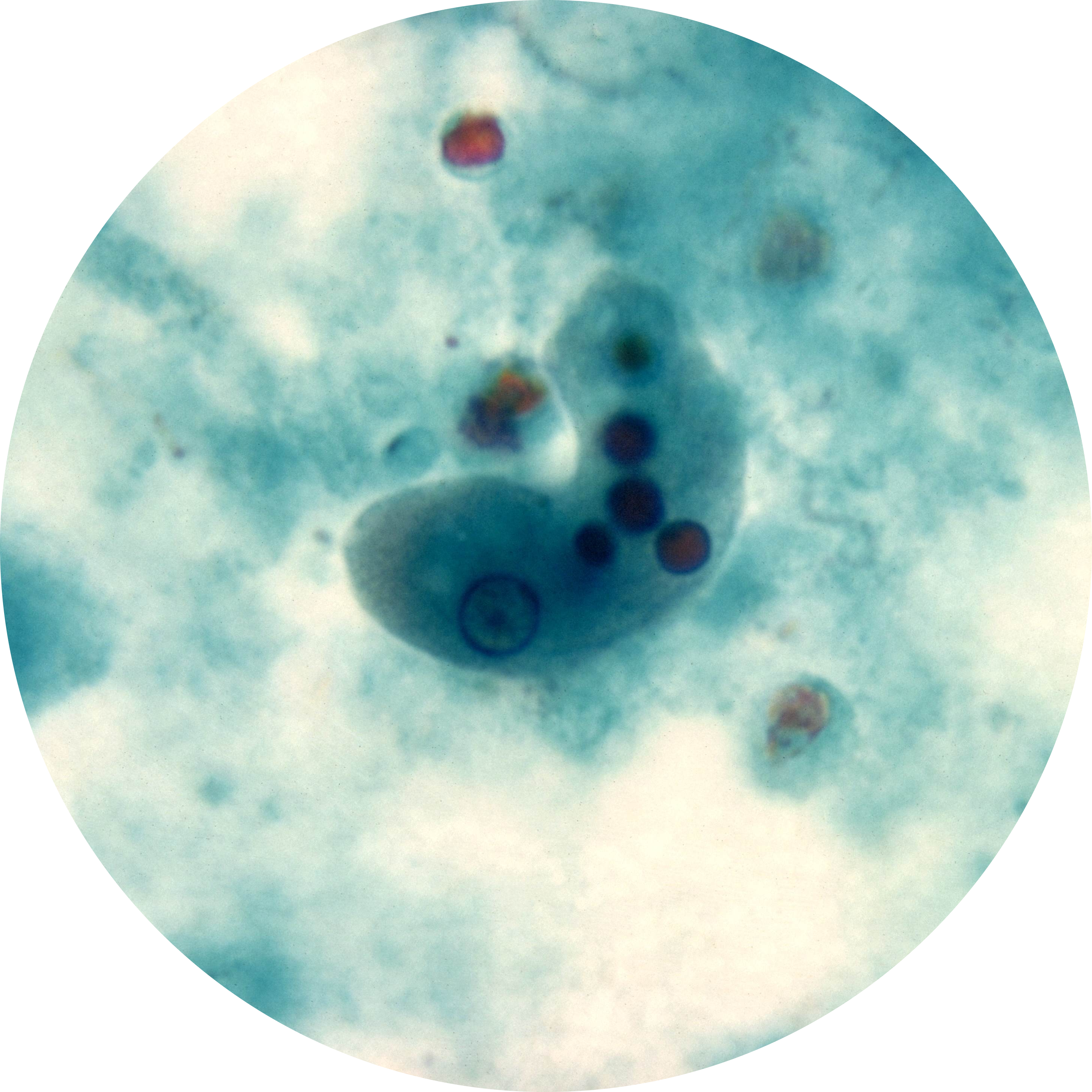
The second line of defense is the intestinal epithelial cell
In the gut, this is done by a specialized epithelial cell (epithelium), which is made up of only one layer. The intestinal mucosa is damaged by SIBO and does not ingest the pathogens due to inflammation; the duct between the intestinal cells remains open, allowing pathogens and toxins to enter the bloodstream, causing inflammation in other parts of the body, in addition to food sensitivities. Allergies develop. If SIBO is not treated for a long time, autoimmune processes may start.
The third line of defense is the gut’s immune system which is 70-80% of all immune cells in the body.
Leakage in the gut can also be caused by gluten, as gluten triggers the production of zonulin in the gut. Zonulin is a protein found in the small intestine that regulates the opening and closing of a channel between intestinal cells. When the zonulin rises, it opens the nodes, and the nodes close when the zonulin level falls down. This protein is activated by gluten, which elevates zonulin and opens nodes in the channels between intestinal cells.
While many suspect celiac diseases as the cause of their problems, SIBO is often the case.
Zonulin can also be activated and elevated by infections such as Candida overgrowth, SIBO, and parasites, and exposure to toxins and stress can all cause leaking intestinal tract.
Symptoms of a leaky gut
- Digestive problems such as bloating, diarrhea, irritable bowel syndrome (IBS)
- Food allergy or food intolerance
- Brain fog, difficulty concentrating, Attention Deficit
- Hyperactivity Disorder (ADD) or Attention Deficit Hyperactivity Disorder (ADHD)
- Mood imbalances such as depression and anxiety, decreased ability to manage stress
- Skin problems such as acne, rosacea, or eczema
- Seasonal allergies or asthma
- Hormonal imbalances such as irregular menstruation, premenstrual syndrome (PMS), or polycystic ovary syndrome (PCOS)
- Diagnosis of autoimmune diseases such as rheumatoid arthritis, Hashimoto’s thyroiditis, lupus, psoriasis, or celiac disease
- Diagnosis of chronic fatigue or fibromyalgia
Causes of a leaky gut
So the following can lead to the development of leaky gut syndrome:
- colonization of harmful pathogens in the intestine
- food allergies
- Hidden food intolerances: these are very insidious because
- intolerance usually develops to food that is consumed often, even every day but does not cause immediate symptoms. (gluten, casein, eggs)
- long-term medication, antibiotics
- digestive enzyme deficiencies
- hormonal changes
- abnormal fluctuations in blood sugar levels
- persistent stress
- Accumulation of chemicals, and toxins in the intestine
10 signs of leaky gut
- Chronic diarrhea, constipation, gas or bloating
- Nutritional deficiencies
- Poor immune system
- Headaches, brain fog, memory loss
- Excessive fatigue
- Skin rashes and problems such as acne, eczema or rosacea
- Cravings for sugar or carbs
- Arthritis or joint pain
- Depression, anxiety, ADD, ADHD
- Autoimmune diseases
If you are experiencing these symptoms, consider talking to your healthcare provider and test your microbiome with the newest technology to find out what is happening inside your gut. Re-rebuilding the gut microbiome and repairing the intestinal wall is essential to stay healthy for the long term.
Resources
- 1] https://pubmed.ncbi.nlm.nih.gov/33171587/
- [2] https://pubmed.ncbi.nlm.nih.gov/32902315/
- [3] https://pubmed.ncbi.nlm.nih.gov/23851019/
- [4] https://pubmed.ncbi.nlm.nih.gov/30394372/