Five facts about SIBO

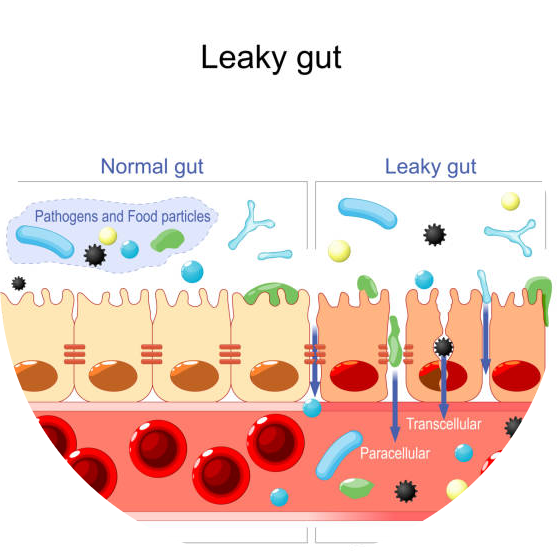
Small Intestinal Bacteria Overgrowth (SIBO) occurs when there are too many bacteria in the small intestine. In this post we will discuss what kind of underlying health concerns may cause bacteria relocation to the small intestine, and we will speak about treatment, relapse and diet as well.
Five facts about SIBO
If we have abdominal complaints, pains, diarrhea, or constipation, we often have to think of SIBO as the primary cause. In this article, you can read the details on the five main facts about SIBO.
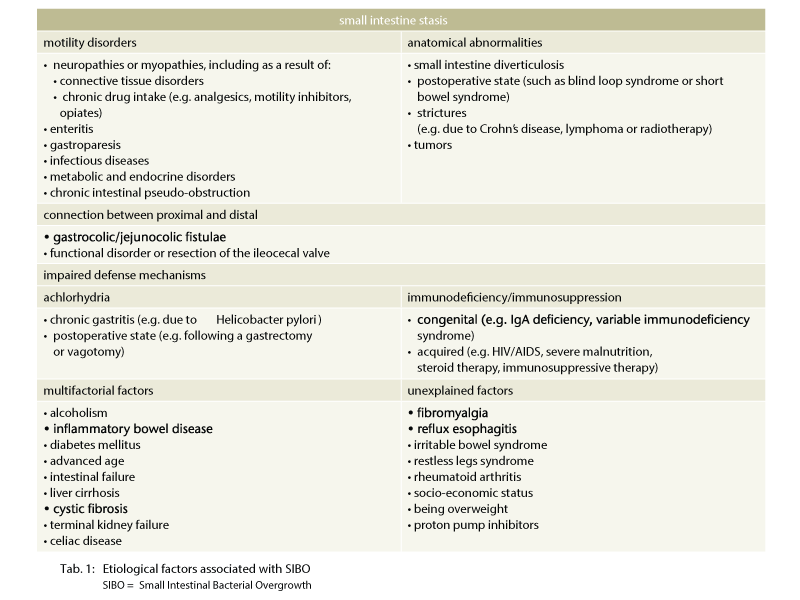
1. SIBO is generally associated with an underlying condition, so it is not an infection, it is a consequence.
There are many reasons why bacteria can relocate to the small intestine. In order to fully treat SIBO, it is important to identify what caused it. Without treating the cause, SIBO will likely recur after treatment.
-
Low stomach acid
Stomach acid kills off many of the microbes that are present in your food, and the environment What causes low acid: Proton Pump Inhibitors – or PPIs. These drugs effectively shut off the production of acid in the stomach. Histamine producing bacteria proliferation in the gut – elevated histamine levels due to these bacteria can cause lower acid levels in the stomach
-
Altered bile flow and enzyme production
Proteolytic enzymes and bile acids are required for adequate digestion of the food and additionally have anti-bacterial effects, helping to protect the gut against bacterial overgrowth. Without sufficient enzymes, carbohydrates may not be broken down sufficiently, providing fuel for bacteria to overgrow. Without the protective effects of enzymes and bile acids, there is an increased risk of developing SIBO (1).
-
Migrating Motor Complex Dysfunction
The migrating motor complex (MMC) is a pattern of gut contraction. Due to this function bacteria are moved from the small intestine into the large intestine between meals and during the night. However, a variety of conditions increase the risk of impaired MMC function, which can lead to SIBO including:
hypothyroidism
opioids PPI’s
Crohn’s, Colitis
Diabetes
Celiac disease
gastroenteritis, (C difficile and other infections)
Lyme disease
The digestive tract requires peristalsis to move food through the digestive tract. If this movement slows down bacteria may colonize in the small intestine. Many conditions can cause slow motility but are not limited to achalasia, gastroparesis, Parkinson’s, scleroderma, and other neurogenic issues (Gut Motility). Additionally, certain medications reduce gut motility such as anticholinergics and opioids (2). Structural changes in the digestive tract can also inhibit the movement of bacteria from the small intestine to the large intestine, or allow migration of bacteria upwards from the large intestine. Including adhesions, obstructions, diverticles), ileocecal valve impairment.
-
Antibiotics and other medication
It is well known that there are medications that affect or interfere with normal intestinal flora. These are mainly antibiotics and antacids. However the non-steroidal anti-inflammatory drugs and steroids also adversely affect the intestinal flora. SIBO can be developed by the dysbiotic effects of antibiotics. Systemic antibiotic exposure kills off both harmful and helpful bacteria, destroying the balance of the microbiome. When many of the protective bacteria are killed, other bacteria can proliferate and overgrow, increasing the risk of developing SIBO. (3).
-
Dysfunctional immune system
The foundation of our gut microbiome is first built in during childbirth and breastfeeding. Children who are born via C-section and those who are not breastfed are at greater risk for microbiome imbalances (dysbiosis)and SIBO (4).
-
Food poisoning
Food poisoning (acute gastroenteritis) can damage the MMC. When we are infected by harmful bacteria during a case of food poisoning, the bacteria release a toxin. Our immune system attacks these toxins. Unfortunately, certain cells in our intestine that play a role in the MMC look very similar to the toxin thus our immune system attacks those cells as well causing damage in the MMC, which can lead to bacterial overgrowth (5, 6).
2. SIBO can be cured but it can relapse, but relapses can be prevented
There may be 2 reasons why you feel relapsed because you have abdominal symptoms again that are reminiscent of SIBO
- The root cause of SIBO is not treated
Check the above underlying issues regarding SIBO and try to find a gastroenterologist who help you find the root cause - You don’t have a relapse, you just have intestinal dysbiosis due to the previous antibiotic treatments. After SIBO treatment it would be obvious to test the gut microbiome to rule out gut dysbiosis
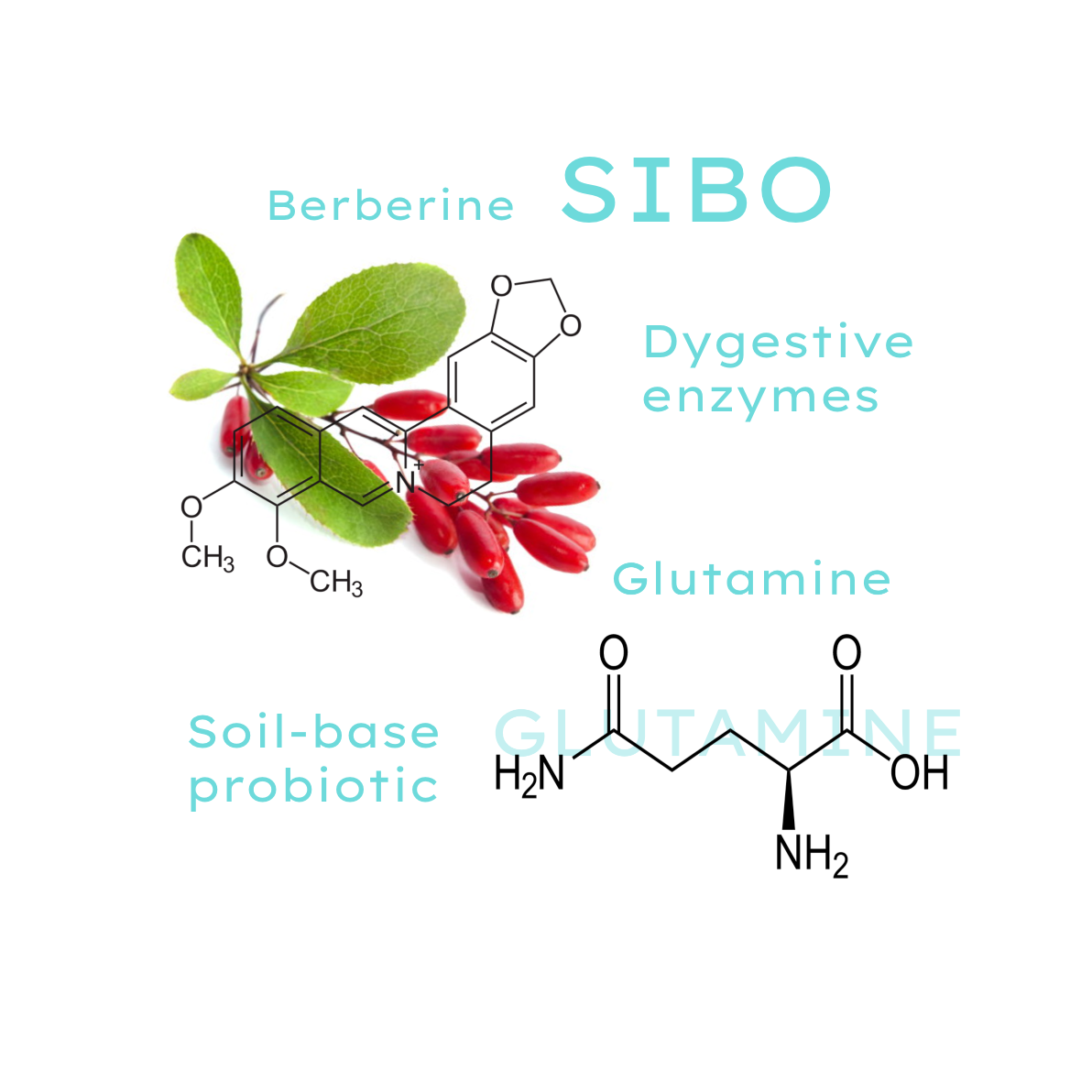
3. If you are having SIBO, soil-based probiotics are recommended to take because they cannot colonize in the small intestine
Soil-based probiotics do not exacerbate symptoms of SIBO. If you have an exacerbation of your symptoms such as more gas, bloating, constipation, diarrhea, or other digestive symptoms after taking probiotics containing any kind of lactobacillus, streptococcus, or bifidobacterium you can be sure that you have SIBO.
This is a strong sign. If you are currently dealing with SIBO, a probiotic containing lactobacillus or bifidobacterium, or streptococcus probiotic strains is not recommended until you eliminate your bacterial overgrowth and repair your gut microbiome.
DO NOT use dietary supplements containing higher amounts of the above probiotic strains to avoid contaminated small intestine (SIBO).
4. Diet will not cure SIBO permanently, it can only relieve the symptoms
Diet is very important. To starve the overgrown bacteria by removing the foods that feed it from your diet is the first step of the SIBO treatment.
This means cutting all sugar and alcohol and limiting carbohydrates such as fruit, starchy vegetables, grains, and legumes. But it won’t be enough!
You need to attack the bacteria because you don’t know how much pathogen is living in your gut. Probably you don’t even know exactly what kind of bacteria is living there. So you will need medication to eliminate SIBO and after treatment, you need to fill your gut with gut bacteria.
5. In case of severe SIBO, you probably need to take antibiotic
If you are struggling with severe SIBO you need to take antibiotics, mainly rifaximin, or that type of antibiotic that was prescribed by your doctor according to the type of SIBO you have.
Herbal antibiotics seem to be as effective as antibiotics but if you have severe long-term symptoms you probably need to take antibiotics first.
Foods in SIBO
Treatment of SIBO
Symptoms and causes of SIBO
Diagnosis of SIBO
SIBO aggravating factors
Resources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2890937/
- https://www.ncbi.nlm.nih.gov/pubmed/7882635
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/
- https://www.ncbi.nlm.nih.gov/pubmed/29018787
- https://www.omicsonline.org/open-access/small-intestinal-bacterial-overgrowth-sibo-2161-069X.1000225.php?aid=31428#8
- https://www.ncbi.nlm.nih.gov/pubmed/25424202
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4430499/
- https://www.ncbi.nlm.nih.gov/pubmed/1634799
- https://www.ncbi.nlm.nih.gov/pubmed/2387510
- https://www.ncbi.nlm.nih.gov/pubmed/9890463
- https://www.ncbi.nlm.nih.gov/pubmed/8853759/
- https://www.ncbi.nlm.nih.gov/pubmed/23270866
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC26223/
- http://www.sciencedirect.com/science/article/pii/S0016508597700751
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2721231/
- http://pediatrics.aappublications.org/content/49/2/233.short
- https://www.hindawi.com/journals/archaea/2014/576249/
- https://www.siboinfo.com/associated-diseases.html