High Homocysteine -The Hidden Dangers and How to Fight Back
One-carbon metabolism is a critical biochemical pathway that plays a pivotal role in cellular function, DNA synthesis, repair, and methylation processes. This metabolic pathway is intricately linked to the availability of B-vitamins, the balance of S-adenosylmethionine (SAMe) and S-adenosylhomocysteine (SAH), homocysteine management, and epigenetic regulation. Optimizing one-carbon metabolism is essential for maintaining overall health and preventing a range of chronic diseases. This article delves into the key components of one-carbon metabolism, including B-vitamin interactions, SAMe/SAH balance, homocysteine management, and epigenetic influences.
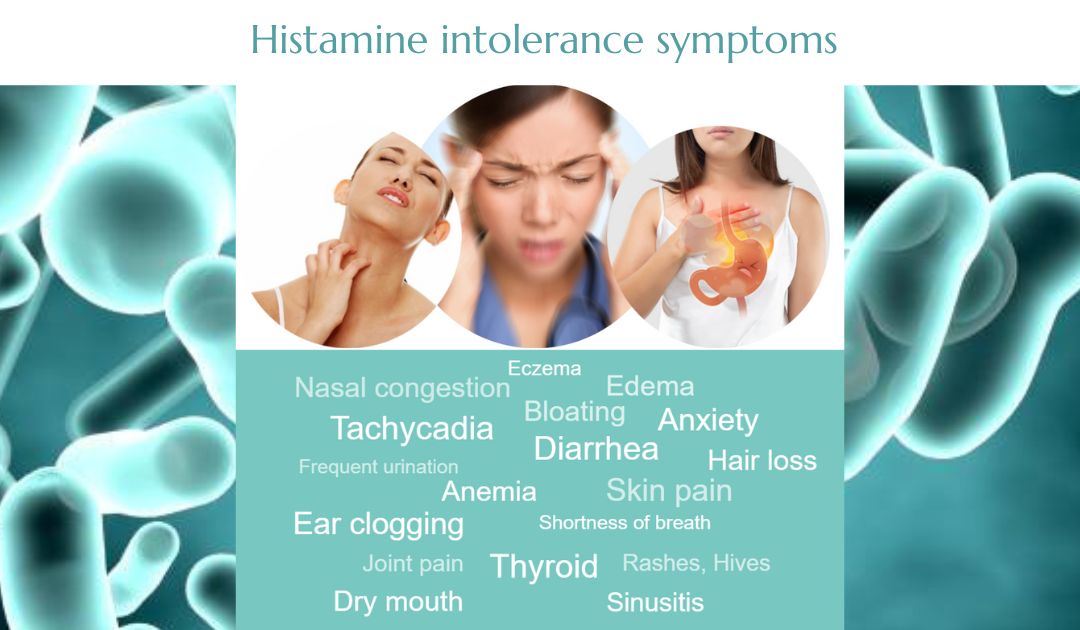
You may not think much about homocysteine, but this little-known amino acid can have a big impact on your health. When levels creep too high, homocysteine becomes a silent threat—damaging blood vessels, increasing inflammation, and raising your risk for heart disease, stroke, and even cognitive decline. The good news? Keeping it in check isn’t as complicated as you might think.
Why Is Homocysteine Dangerous?
Think of homocysteine as a metabolic byproduct that needs to be processed efficiently. Under ideal conditions, your body recycles it into methionine (a useful amino acid) or converts it into cysteine (which supports detoxification and antioxidant defense). But when these pathways don’t function properly—due to vitamin deficiencies, genetic mutations (like MTHFR), or lifestyle factors—homocysteine builds up, wreaking havoc on your cardiovascular and neurological health.
1. B-Vitamin Interactions in One-Carbon Metabolism
B-vitamins are essential cofactors in one-carbon metabolism, facilitating the transfer of one-carbon units for various biochemical reactions. The primary B-vitamins involved include folate (B9), vitamin B12 (cobalamin), vitamin B6 (pyridoxine), and riboflavin (B2).
Folate (Vitamin B9)
Folate is a cornerstone of one-carbon metabolism, serving as a carrier of one-carbon units. It is converted into tetrahydrofolate (THF), which participates in the synthesis of purines, thymidylate, and the remethylation of homocysteine to methionine. The enzyme methylenetetrahydrofolate reductase (MTHFR) plays a crucial role in converting 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate, the active form of folate required for homocysteine remethylation.
Vitamin B12 (Cobalamin)
Vitamin B12 is a cofactor for methionine synthase, the enzyme that catalyzes the conversion of homocysteine to methionine using 5-methyltetrahydrofolate as a methyl donor. A deficiency in vitamin B12 can lead to elevated homocysteine levels and impaired methylation processes.
Vitamin B6 (Pyridoxine)
Vitamin B6 is involved in the transsulfuration pathway, where it acts as a cofactor for cystathionine β-synthase (CBS) and cystathionine γ-lyase (CGL). These enzymes convert homocysteine to cysteine, which is further metabolized to glutathione, a critical antioxidant.
Riboflavin (Vitamin B2)
Riboflavin is a precursor for flavin adenine dinucleotide (FAD), a cofactor for MTHFR. Adequate riboflavin levels are necessary for optimal MTHFR activity and efficient folate metabolism.
Interplay Between B-Vitamins
The B-vitamins work synergistically in one-carbon metabolism. For instance, a deficiency in one B-vitamin can impair the function of others. For example, vitamin B12 deficiency can lead to functional folate deficiency by trapping folate in the form of 5-methyltetrahydrofolate, a phenomenon known as the “methyl trap hypothesis.”
2. SAMe/SAH Balance: The Methylation Cycle
The balance between S-adenosylmethionine (SAMe) and S-adenosylhomocysteine (SAH) is a critical determinant of cellular methylation capacity. The supplement SAMe is the universal methyl donor for over 200 methylation reactions, including DNA, RNA, protein, and lipid methylation.
SAMe Synthesis
SAMe is synthesized from methionine and ATP via the enzyme methionine adenosyltransferase (MAT). The availability of methionine, derived from the remethylation of homocysteine, is thus crucial for SAMe production.
SAH Formation
After donating a methyl group, SAMe is converted to SAH, which is a potent inhibitor of methyltransferases. SAH is subsequently hydrolyzed to homocysteine and adenosine by the enzyme SAH hydrolase.
SAMe/SAH Ratio
The SAMe/SAH ratio is a key indicator of cellular methylation status. A high SAMe/SAH ratio promotes methylation, while a low ratio inhibits it. Factors that influence this ratio include the availability of B-vitamins, the activity of enzymes involved in the methylation cycle, and the efficiency of homocysteine remethylation and transsulfuration.
3. Homocysteine Management: A Central Player
Homocysteine is a sulfur-containing amino acid at the crossroads of one-carbon metabolism. Elevated homocysteine levels, known as hyperhomocysteinemia, are associated with an increased risk of cardiovascular disease, cognitive decline, and other chronic conditions.
Remethylation Pathway
Homocysteine can be remethylated to methionine via two pathways: the folate-dependent pathway, which requires 5-methyltetrahydrofolate and vitamin B12, and the betaine-dependent pathway, which uses betaine as a methyl donor.
Transsulfuration Pathway
Alternatively, homocysteine can be converted to cysteine via the transsulfuration pathway, which requires vitamin B6. This pathway not only reduces homocysteine levels but also contributes to the synthesis of glutathione, a critical antioxidant.
Factors Influencing Homocysteine Levels
Several factors can influence homocysteine levels, including genetic polymorphisms (e.g., MTHFR C677T), dietary intake of B-vitamins, renal function, and lifestyle factors such as smoking and alcohol consumption.
4. Epigenetic Influences: DNA Methylation and Beyond
One-carbon metabolism has profound implications for epigenetics, particularly DNA methylation, which is the addition of a methyl group to the cytosine base in DNA, typically at CpG dinucleotides.
DNA Methylation
DNA methylation is a key epigenetic mechanism that regulates gene expression. SAMe serves as the methyl donor for DNA methyltransferases (DNMTs), which catalyze the transfer of a methyl group to DNA. Aberrant DNA methylation patterns, such as global hypomethylation or gene-specific hypermethylation, are associated with various diseases, including cancer, cardiovascular disease, and neurodegenerative disorders.
Histone Methylation
In addition to DNA methylation, SAMe is also involved in histone methylation, which affects chromatin structure and gene expression. Histone methyltransferases (HMTs) use SAMe to methylate specific lysine or arginine residues on histone proteins, influencing transcriptional activity.
Epigenetic Regulation by B-Vitamins
B-vitamins play a crucial role in maintaining epigenetic integrity. For example, folate and vitamin B12 are essential for the synthesis of SAMe, while vitamin B6 is involved in the regulation of histone methylation. Deficiencies in these vitamins can lead to epigenetic dysregulation, contributing to disease pathogenesis.
Transgenerational Epigenetic Effects
Emerging evidence suggests that one-carbon metabolism and epigenetic modifications can have transgenerational effects. Maternal nutrition, particularly B-vitamin status, can influence the epigenetic programming of the offspring, potentially affecting their health outcomes later in life.
5. How to Keep Homocysteine Levels in Check
- Load Up on B-Vitamins
B6, B9 (folate), and B12 are essential for breaking down homocysteine. Without them, this harmful amino acid accumulates in the bloodstream. To stay on top of your B-vitamin intake, include leafy greens, eggs, fish, and legumes in your diet. If you have an MTHFR mutation, consider supplementing with methylated forms of folate and B12 for better absorption. - Support Your Detox Pathways
The transsulfuration pathway helps clear homocysteine by converting it into cysteine, a precursor to glutathione—your body’s master antioxidant. Foods rich in sulfur (like garlic, onions, and cruciferous vegetables) can support this process and enhance detoxification. - Reduce Inflammatory Triggers
Chronic inflammation and oxidative stress can worsen homocysteine-related damage. Cut back on processed foods, sugar, and alcohol while increasing your intake of omega-3s (found in fatty fish, walnuts, and flaxseeds). - Stay Active
Exercise isn’t just great for your heart—it also helps regulate homocysteine levels by improving circulation and metabolic efficiency. Even 30 minutes of moderate activity daily can make a difference. - Get Tested Regularly
If you have a family history of heart disease, migraines, or cognitive issues, ask your doctor to check your homocysteine levels. A simple blood test can reveal whether you need to make dietary or lifestyle changes.
6. Strategies for Optimizing One-Carbon Metabolism
Optimizing one-carbon metabolism requires a multifaceted approach that addresses dietary, genetic, and lifestyle factors.
Dietary Interventions
A diet rich in B-vitamins is essential for optimal one-carbon metabolism. Foods high in folate (e.g., leafy greens, legumes), vitamin B12 (e.g., animal products), vitamin B6 (e.g., poultry, fish), and riboflavin (e.g., dairy, eggs) should be prioritized. In cases of deficiency or increased demand (e.g., pregnancy, aging), supplementation may be necessary.
Genetic Considerations
Genetic polymorphisms, such as the MTHFR C677T variant, can affect enzyme activity and nutrient requirements. Personalized nutrition, based on genetic testing, can help tailor interventions to individual needs.
Lifestyle Modifications
Lifestyle factors, such as smoking cessation, moderate alcohol consumption, and regular physical activity, can positively influence one-carbon metabolism. Stress management and adequate sleep are also important for maintaining metabolic balance.
Monitoring Biomarkers
Regular monitoring of biomarkers, such as homocysteine levels, SAMe/SAH ratio, and methylation status, can provide valuable insights into one-carbon metabolism and guide interventions.
7. Here are natural compounds that help regulate homocysteine levels
1. Betaine Anhydrous (Trimethylglycine, TMG)
- Function: Acts as a methyl donor in the remethylation of homocysteine to methionine via the betaine-homocysteine methyltransferase (BHMT) pathway.
- Justification: Helps reduce homocysteine levels, especially in individuals with MTHFR mutations or impaired folate metabolism.
2. Riboflavin (Vitamin B2)
- Function: Essential for the activation of methylenetetrahydrofolate reductase (MTHFR), the enzyme that converts folate into its active form for homocysteine metabolism.
- Justification: Supports folate metabolism and homocysteine conversion, particularly in individuals with MTHFR gene variants.
3. Pyridoxine (Vitamin B6)
- Function: A crucial cofactor in the transsulfuration pathway, where homocysteine is converted into cysteine and then glutathione (a key antioxidant).
- Justification: Helps break down homocysteine into beneficial compounds, reducing its accumulation.
4. Folate (Vitamin B9, Methylfolate, or Folinic Acid)
- Function: Supports homocysteine remethylation into methionine, particularly when in its active 5-MTHF (methylfolate) form.
- Justification: Essential for homocysteine metabolism; deficiencies are strongly linked to elevated homocysteine levels.
5. S-Adenosylmethionine (SAM-e)
- Function: A key methyl donor in numerous biological processes; indirectly supports homocysteine metabolism by maintaining methylation balance.
- Justification: Helps maintain a healthy SAMe/SAH (S-adenosylhomocysteine) ratio, reducing homocysteine accumulation.
6. Cobalamin (Vitamin B12, Methylcobalamin or Hydroxocobalamin)
- Function: Works with folate to convert homocysteine back into methionine via the methionine synthase enzyme.
- Justification: Deficiencies lead to homocysteine buildup, making adequate B12 intake crucial for maintaining normal levels.
A combination of Betaine, B2, B6, Folate, SAM-e, and B12 works synergistically to lower homocysteine levels through methylation, transsulfuration, and enzyme activation. Addressing deficiencies in these nutrients can help reduce the risk of cardiovascular disease, cognitive decline, and other homocysteine-related health issues.
Conclusion
One-carbon metabolism is a complex and dynamic pathway that integrates nutrient metabolism, methylation processes, and epigenetic regulation. Optimizing this pathway through adequate B-vitamin intake, maintaining SAMe/SAH balance, managing homocysteine levels, and understanding epigenetic influences is crucial for overall health and disease prevention. A holistic approach that considers dietary, genetic, and lifestyle factors is essential for achieving optimal one-carbon metabolism and promoting long-term well-being.
Final Thoughts: Small Changes, Big Impact
Homocysteine may be a silent killer, but you don’t have to be its victim. By optimizing your diet, supporting methylation, and adopting a healthy lifestyle, you can keep this amino acid in check—protecting your heart, brain, and longevity. The power is in your hands!